Division of Coronary Diseases
Target disease,treatment
Major Diagnostic Services and Therapeutic Modalities
Diagnostic Services
- Resting and stress echocardiography
- Cardiac magnetic resonance imaging (MRI)
- Coronary computed tomography (CT)
- Coronary angiography
- Coronary intravascular ultrasound, optical coherence tomography, and vascular endoscopy
Therapeutic Modalities
- Pharmacotherapy (e.g., β-blockers, calcium channel blockers, nitrates, antiplatelet medications, and statins)
- Percutaneous coronary intervention (balloon angioplasty and stenting) and mechanical circulatory support
- Cardiac rehabilitation and other physical activity programs
1. Reperfusion for Acute Myocardial Infarction
Acute myocardial infarction frequently develops when a coronary atherosclerotic plaque ruptures and the resultant thrombus blocks blood flow. The most critical step in treating patients with acute myocardial infarction is to rapidly establish blood flow to tissue (coronary recanalization).
- Please click here for a summary of clinical outcomes for acute myocardial infarction at NCVC Hospital.
Staff members are on-call around the clock in NCVC Hospital's emergency care unit, which performs approximately 200 cardiac catheterizations each year. As a national model for emergency medical services, ambulances are equipped with an advanced mobile telemedicine system that allows real-time transmission of electrocardiographic and other data via the Internet. The mobile telemedicine system minimizes the time lag from disease onset to diagnosis and treatment. As a result, growing numbers of patients seek help at NCVC Hospital; most patients survive to discharge. NCVC Hospital achieved annual in-hospital mortality rates below 5% in recent years, including in 2015.
Figure 1. Annual NCVC Hospital in-hospital mortality rates from 1978 to 2015
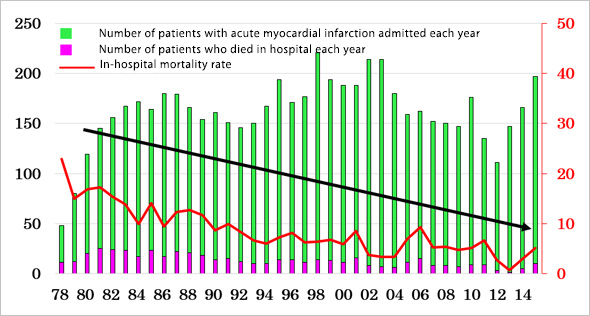
Figure 2. Examples of acute myocardial infarction treatment
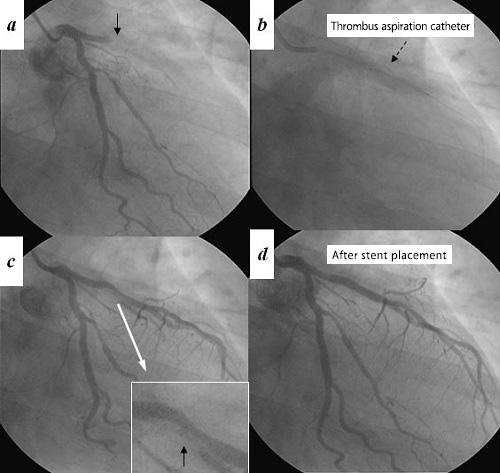
- a. Coronary angiograph taken in a patient with acute anterior wall myocardial infarction showing proximal occlusion of the left anterior descending artery (black arrow).
- b. An aspiration catheter was inserted to remove the thrombus from the occluded vessel.
- c. Removal of the thrombus achieved reperfusion in the presence of residual atherosclerotic stenosis and ruptured plaque.
- d. Stent placement and dilation successfully relieved the stenosis and restored blood flow.
2. Emergency Cardiovascular Care
Many cardiovascular disorders need prompt medical attention after symptom onset. Delays in treatment may lead to rapid deterioration or death. Examples of such conditions include ischemic diseases (e.g., acute myocardial infarction and unstable angina), acute cardiac failure, severe pulmonary vascular disorders, severe arrhythmias, and acute aortic diseases.
The NCVC Hospital's Cardiovascular Care Unit (CCU) hosts a team of experts specialized in cardiac intensive care and emergency medicine. They provide emergency care 24 hours a day throughout the year.
In patients with serious circulatory problems, the heart can no longer distribute blood around the body properly (pump failure). This leads to decreased blood pressure, multiple organ failure, and ultimately death due to blood and nutrient shortage. If catheterization and medications cannot improve cardiac function, mechanical support is needed to assist circulation. Typical examples include intraaortic balloon pumping (IABP, Figure 3A) and percutaneous cardiopulmonary support (PCPS, Figure 3B). The catheters for these support devices can be readily advanced into position. Combined with medications, these techniques can improve heart function.
If pump failure or cardiac arrest interrupts blood supply to the brain even for a relatively short period of time, the brain may be damaged irreversibly (hypoxic encephalopathy). Recent international studies have shown that therapeutic controlled hypothermia reduces the risk of death and permanent disability in patients with hypoxic encephalopathy. At NCVC Hospital, therapeutic hypothermia involving surface cooling pads and PCPS is routinely used in combination with cardiac treatments.
Figure 3A. Intraaortic balloon pumping (IABP)
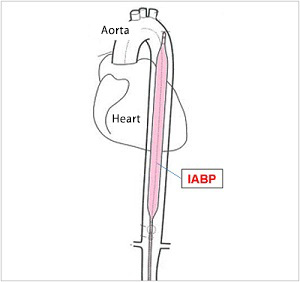
A key advantage of IABP is its ease of use. A balloon placed in the descending aorta can help decrease cardiac burden.
Figure 3B. Percutaneous cardiopulmonary support (PCPS)
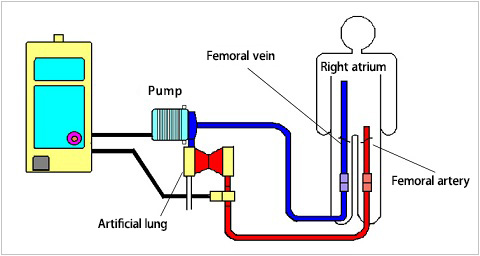
PCPS provides powerful circulatory support for patients with severe pump failure or in cardiac arrest. Generally, the drainage catheter is inserted percutaneously into the right atrium via the right femoral vein. The blood is oxygenated as it passes through the artificial lung and is subsequently pumped back into the body. The oxygenated blood is typically returned via a femoral artery cannula. Oxygenated blood in the upper body flows retrograde through the aorta, competing with native cardiac output.
3. Cardiovascular Imaging, Catheterization, and Pharmacotherapy
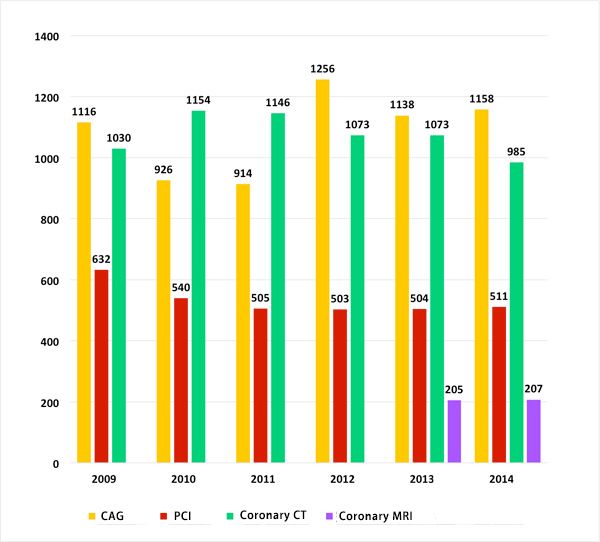
The Division of Coronary Diseases employs computed tomography (CT), magnetic resonance imaging (MRI), radioisotope scanning, and other non-invasive or minimally invasive modalities to diagnose cardiovascular disorders. The Division is especially committed to outpatient CT screening for coronary artery disease (Figure 4). Approximately 2,000 persons undergo coronary CT angiography screening each year at NCVC Hospital. For percutaneous coronary intervention (PCI), the Division of Coronary Diseases offers a variety of advanced treatment options, including rotational atherectomy (rotablation) and drug-eluting stent implantation. In rotablation, a tiny fast-rotating diamond-coated drill is introduced to chip away calcified plaques. Drug-eluting stents are designed to prevent restenosis by gradually releasing single or multiple pharmaceutical agents into the bloodstream and surrounding tissue. The timing of PCI is optimized based on the results of cardiovascular imaging and vascular function tests. After PCI, the risk of disease recurrence and aggravation is minimized using antiatherosclerotic drugs.
Conventionally, catheter angiography was employed for evaluating coronary artery abnormalities. In recent years, CT angiography has been gaining popularity. In addition to these techniques, NCVC Hospital is using coronary MRI angiography, a diagnostic tool for evaluating plaque vulnerability (Figure 5). This imaging modality is noninvasive and free from exposure to ionizing radiation and contrast agents. Coronary MRI angiography is effective for predicting future risk of cardiac events and preventing perioperative myocardial injury from coronary catheterization.
Figure 4. Coronary CT angiography
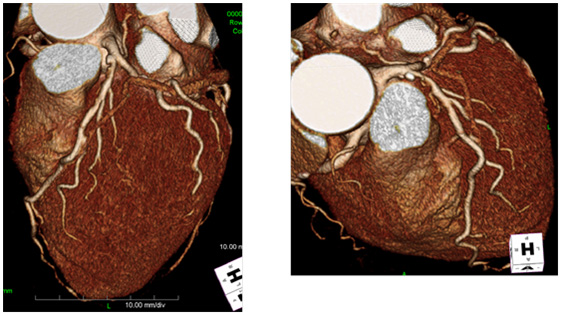
Figure 5. Number of patients who underwent PCI, catheter angiography (CAG), coronary CT angiography, and coronary MRI angiography at NCVC Hospital from 2009 to 2014
4. Cardiac Rehabilitation
NCVC Hospital has cardiac rehabilitation programs. These programs include exercise therapy, patient education, lifestyle guidance, and counseling services. These are designed to help patients to recover physical strength, prepare themselves mentally and emotionally for returning to the community and work life, prevent disease recurrence, and maintain quality of life. These programs are particularly helpful for patients with heart failure or after cardiac surgery.
- For details about the Division of Cardiovascular Rehabilitation, please click here.
- For details about cardiac rehabilitation programs, please click here.
last updated : 2021/10/01
