Division of Cerebrovascular Medicine and Neurology
More details
- Clinical Team: Cerebrovascular Medicine (Brain medicine A)
What We Do
Strokes or cerebrovascular accidents occur frequently in Japan. They are the third leading cause of death, accounting for the fourth largest share of the total national health care expenditures and the greatest proportion of elderly health care costs. With the advent of the ageing society, the number of stroke victims is escalating each year together with an increasing number of patients with lifestyle-related diseases. Stroke represents one of the greatest cardiovascular challenges for health care providers in Japan. The Division of Cerebrovascular Medicine and Neurology regards stroke as a systemic vascular disorder and provides an integrated treatment approach involving neurology, cardiovascular medicine, emergency medicine, the science of thrombosis and hemostasis, and rehabilitation medicine. In close cooperation with other departments and sections related to cardiovascular and atherosclerotic diseases, including neurosurgery, brain rehabilitation, diagnostic radiology, and nursing, we are committed each day to diagnosis, treatment, investigation, research, education, and enlightenment to overcome cerebrovascular disorders (e.g., cerebral infarction and hemorrhage).
Staff Members
Our Division has approximately 40 physicians, including 16 senior staff members (e.g., division head and chief physicians), 18 specialists in training and junior physicians with a 3- to 5-year career, and a few ad-hoc trainees. Our Division consists of two groups: Cerebrovascular Medicine (Brain Medicine A) and Neurology (Brain Medicine B). Both groups are devoted to stroke diagnosis, treatment, research, and education. Both groups provide the latest medical services. Patients with an acute stroke will be attended to by physicians from both groups.
Medical Services
We provide acute care for patients with cerebrovascular diseases (e.g., stroke and brain hemorrhage) and related neurological disorders. Outpatient services are available in the morning and afternoon from Monday through Friday. Patients visiting our Division for the first time are seen by a head or chief physician. Return-visit patients are taken care of in the specialty outpatient clinic that hosts four full-time physicians. To address emergency situations, physicians are on call around the clock throughout the year.
Our Division emphasizes the latest techniques for stroke care. Patients with an acute stroke are admitted to the Stroke Care Unit (SCU) for intensive treatment. NCVC Hospital's SCU was the first of its kind established in Japan, and it now has 23 beds. This capacity is large enough to accommodate acute patients at any time. The annual number of SCU patients at our hospital is increasing every year, with decreasing mortality trends. We are proud that our clinical outcomes rival those of the world's leading acute care facilities. Table 1 summarizes our clinical results in acute stroke and brain hemorrhage patients over the past 3 years. These results are comparable to or better than those of other SCUs in Japan.
Since intravenous tissue plasminogen activator (tPA) therapy was approved in 2005 for treating acute strokes in Japan, the role of multidisciplinary team care has been increasing its significance in stroke management. NCVC Hospital has developed a comprehensive, integrated approach to acute care and safely administers tPA therapy in an average of four patients per month. NCVC Hospital administered tPA therapy in a total of 325 patients as of August 2012 (approximately 7 years after approval), and no adverse sequelae were observed in nearly half of them at 3 months after stroke onset. These results are among the best in Japan (Figures 2 and 3). Although NCVC Hospital admits patients with serious conditions more frequently than other acute stroke centers, it has produced excellent clinical outcomes, with more than 95% of acute stroke patients surviving 1 month after symptom onset.
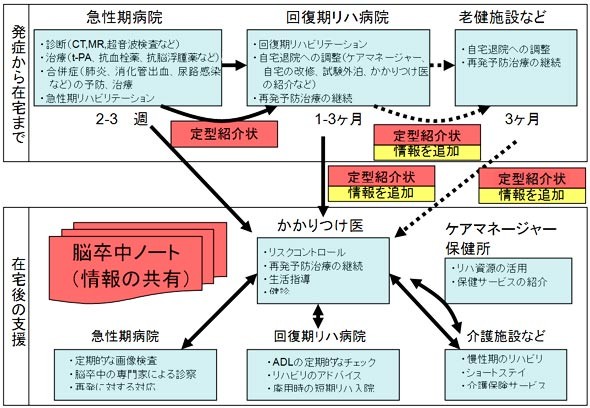
When their condition stabilizes after treatment at the SCU, patients are transferred to the general stroke ward (approximately 80 beds) and start rehabilitation exercises and other postacute therapy in preparation for discharge. NCVC Hospital serves as a hub stroke center for Toyono Region, Osaka. The coordination of and partnerships with stroke-related service providers allow for a seamless array of health care ranging from acute treatment to in-home support (local stroke network pathway), as shown in Figure 4. Moreover, we identify patients who need surgical treatment (e.g., invasive operation or endovascular therapy) and refer them to the Division of Neurosurgery without delay.
Figure 1. Changes over time in the number of patients admitted to the SCU and in-hospital mortality
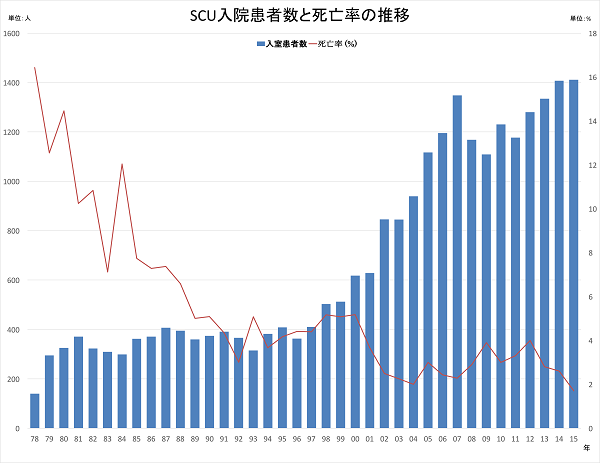
Table 1. Clinical outcomes of NCVC Hospital from 2011 to 2013
| Year | |||
|---|---|---|---|
| 2011 | 2012 | 2013 | |
| Number of admitted acute stroke patients | 550 | 626 | 594 |
| Proportion of patients with severe condition (NIHSS ≥ 8), % |
35 | 36 | 34 |
| Proportion of patients with independence in self-care at discharge (mRS score 0-2), % |
55 | 52 | 59 |
| Number of admitted brain hemorrhage patients | 192 | 208 | 252 |
| Proportion of patients with severe condition (NIHSS ≥ 8), % |
70 | 79 | 70 |
| Proportion of patients with independence in self-care at discharge (mRS score 0-2), % |
28 | 18 | 24 |
| Number of admitted patients with transient ischemic stroke | 97 | 110 | 103 |
NIHSS, National Institutes of Health Stroke Scale; mRS, modified Rankin Scale.
Treatment
| Year | |||
|---|---|---|---|
| 2011 | 2012 | 2013 | |
| Number of patients treated with tPA | 58 | 69 | 78 |
| Proportion of patients with independence in self-care at discharge (mRS score 0-2), % |
41 | 51 | 49 |
| Number of patients transferred through the local stroke network pathway | - | 406 | 434 |
| Number of patients who underwent acute endovascular therapy (e.g., with Merci or Penumbra system) |
9 | 21 | 42 |
Diagnostic Imaging Scans
| Number of patients who underwent: | Year | ||
|---|---|---|---|
| 2011 | 2012 | 2013 | |
| Carotid ultrasound | 5,171 | 4,807 | 5,474 |
| Transcranial ultrasound | 763 | 626 | 642 |
| Cerebral angiography | 120 | 181 | 139 |
Figure 2. Clinical outcomes of intravenous tPA therapy
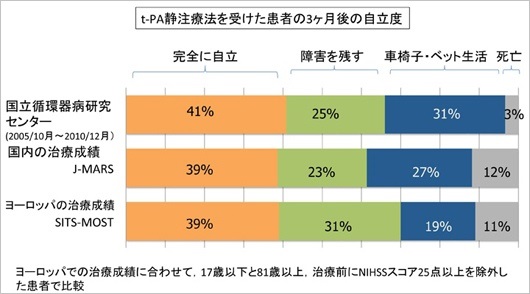
Among patients treated at NCVC Hospital, 41% achieved complete independence (modified Rankin scale score 0 or 1). NCVC Hospital has better clinical outcomes than other facilities in Japan and overseas (<40%).
Figure 3. Intravenous tPA time window extended to 4.5 hours
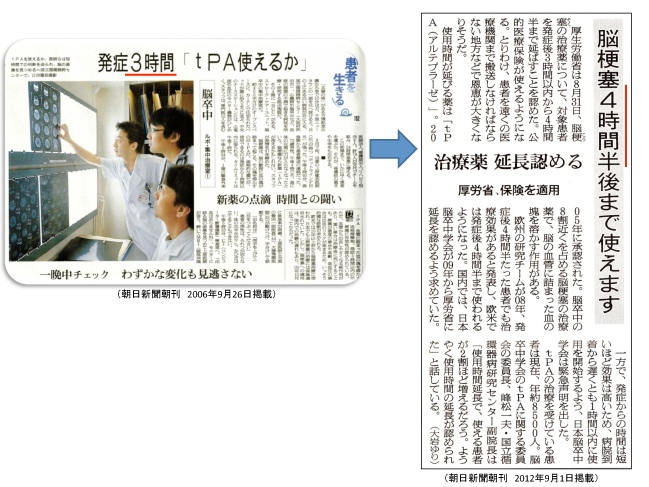
Figure 4. Toyono Local Stroke Network
Clinical Research
NCVC Hospital is actively engaged in clinical research for primary and secondary stroke prevention, development of new diagnostic and treatment modalities for acute cerebral vascular injury, and multicenter clinical trials of acute stroke. NCVC Hospital is also developing regenerative medicine and other cutting-edge treatment methods. For details of our research activities, please visit the Cerebrovascular Medicine (Brain Medicine A) and Neurology (Brain Medicine B) pages.
Postgraduate Medical Training
Whereas major advancements have been made in acute stroke care, including the development of intravenous thrombolytic agents and national health insurance coverage of stroke care unit services, a huge gap exists in the number of physicians who provide stroke care. Charged with the mission to foster practitioners, researchers, and educators in the field of acute and postacute stroke care, our Division actively invites junior physicians to receive education and training. In addition to the latest technologies and skills in stroke care, our curriculum covers a wide range of disciplines including cardiology, neurology, nephrology, cardiovascular medicine, endocrinology, emergency medicine, and rehabilitation. We encourage junior physicians to participate in prospective clinical studies and trials and to publish their findings at national and international conferences and journals.
last updated : 2021/10/05
