Division of Cerebrovascular Medicine and Neurology
Target disease,treatment
Target Conditions
We provide medical care for patients who experience an acute stroke.
For more details, please refer to: What is a stroke?
Cerebral Infarction
Cerebral thrombosis is a condition in which a blood clot (thrombus) forms in a narrowed atherosclerotic cerebral artery and thereby blocks its blood supply. A cerebral embolism develops when a blood clot or other substance formed in the heart or other sites (embolus) travels into the brain and clogs an artery. Cerebral thrombosis commonly develops in the elderly population, characterized by a gradual progression of cognitive, locomotive, and consciousness disturbance. A cerebral embolism most commonly presents with a sudden onset of speech disturbance and arm or leg numbness, especially on one side of the body. These symptoms require immediate medical attention.
Transient Ischemic Attack
- Transient Ischemic Attack (TIA) Care at NCVC Hospital
A transient ischemic attack (TIA) is a temporary interruption of cerebral blood flow due to thrombosis or embolism. Although symptoms of a TIA may disappear within minutes to an hour, TIA is a warning sign of cerebral infarction. Patients suspected of experiencing a TIA cannot wait for treatment. They should immediately undergo examinations and receive treatment for the cause.
Intracerebral Hemorrhage
An intracerebral hemorrhage is bleeding from a ruptured artery within the brain, frequently observed in patients with hypertension. In many cases, patients experience a sudden onset of consciousness disturbance, hemiplegia, difficulty speaking, and a rise in blood pressure. These conditions indicate a need for immediate action.
Asymptomatic Cerebrovascular Damage and Asymptomatic Carotid Stenosis
Some patients may develop a cerebral infarction or intracranial bleeding while they are unaware of any signs or symptoms. In addition, patients with carotid stenosis may feel no symptoms, although it predisposes them to the risk of cerebral infarction. Patients with these conditions should be assessed for the cause to eliminate the risk of stroke.
For further information on strokes, please refer to the following pages:
- Types of and measures against strokes
- What to do when a stroke develops
- Stroke and speech disturbance
- Keys for preventing a stroke
- Tips for stroke prevention
Major Diagnostic Methods
For further details, please refer to: What does a brain scan image show?
Head Computed Tomography (CT)
CT scans use x-ray radiation to determine the presence or absence of a stroke. Because a CT scan itself takes only a few minutes, this is the first-choice diagnostic imaging technique for patients suspected of having a stroke.
Head Magnetic Resonance Imaging (MRI) and Magnetic Resonance Angiography (MRA)
MRI and MRA scans use a powerful magnetic field and yield more detailed information than CT scans. CT scans may fail to detect lesions of cerebral infarction if taken immediately after the onset of symptoms. On the other hand, MRI scans can detect focal lesions as early as 30 minutes after symptom onset. MRA provides images of the blood vessels within the brain. An MRA takes approximately 15 minutes to complete, requiring a longer amount of time than CT. MRA scans cannot be done for patients with pacemakers or metal implants.
Vascular Sonography: Carotid Artery, Intracranial Vessels, and Lower-Limb Veins
Vascular sonography uses ultrasound waves to investigate the blood vessel. This noninvasive test can be readily conducted at the bedside to scan for blockade and narrowing of head and neck vessels. Ultrasonography of lower-limb veins can also be conducted to check for the possibility of lower-limb thrombi entering and clogging cerebral blood vessels.
Transthoracic and Transesophageal Echocardiography
Echocardiography produces images of the heart using ultrasound. It may be performed by placing a transducer on the surface of the chest (transthoracically) or by inserting a transducer into the esophagus (transesophageally). The heart and its vessels assume an important part of cerebral infarction risk because emboli from the heart and aorta may enter and block brain arteries.
Catheter Angiography
Catheter angiography can provide the most detailed information on the condition of a blood vessel (e.g., narrowing and occlusion). A small catheter tip is advanced into the blood vessel of concern (e.g., cerebral or carotid artery). A contrast medium is injected from the catheter tip to enhance imaging capabilities. This imaging modality allows for subsequent endovascular therapy to remove clots and expand narrowed vessels.
Nuclear Imaging: Single Photon Emission Computed Tomography (SPECT) and Positron Emission Tomography (PET)
These examinations use radioisotopes to investigate cerebral blood flow and metabolism in depth. These scans can show the degrees of cerebral blood flow and perfusion in patients with arterial stenosis or occlusion.
Expanding the treatment time window -RAPID-
We are proud to announce that we are the first center in Japan to install RAPID, a fully automated perfusion image analysis software, from 2017. Recent studies demonstrated that acute ischemic stroke patients with a perfusion – core mismatch1) with a certain volume of penumbra2) responds well to reperfusion therapy even beyond the time window as before. American Stroke Association Guidelines and European Stroke Guidelines has referred to the use of RAPID for the efficacy of treatment up to 24 hours. Currently, the froth edition of the Japanese Guidelines for Mechanical Thrombectomy has also noted this information.
Real-time analysis of cerebral perfusion images is necessary to determine which patients are eligible for exptended treatment time, and RAPID is considered to be the most evidence-based software in use worldwide. By analyzing cerebral perfusion images within 24 hours, patients with acute cerebral infarction who are beyond the conventional treatment time frame may be eligible for treatment if there is a mismatch2).
<Figure 1>
CT perfusion analysis of acute ischemic stroke by RAPID.
The left cerebral infarction (left image; pink) is automatically calculated as a volume of 6 ml. The green image on the right side of the figure, which shows abnormal cerebral perfusion, is volumetrically calculated as 82 ml, and illustrates that this area is a penumbra that can be salvageable. If the ratio of pink to green is greater than 1.8, we call this a target mismatch, and the patient will respond well to reperfusion therapy. In this case, although the onset to arrival was was 10 hours, the ratio was 14, and the patient responded well to reperfusion therapy.
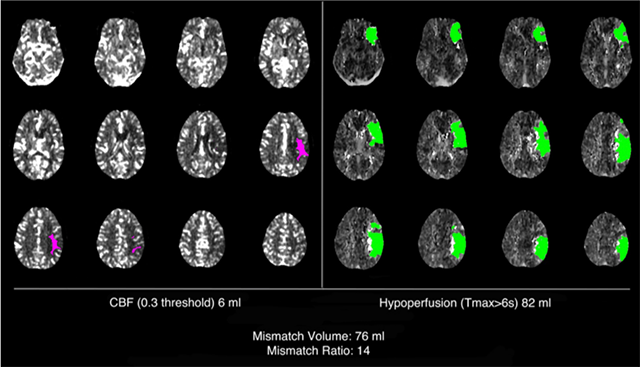
From RAPID web site
<Annotation>
1) Perfusion – core mismatch
The high ratio between the infarction core (high-signal area on MRI DWI or low CBF in CT perfusion) and the penumbra area would indicate the potential of salvageable brain tissue, which the symptom may progress if reperfusion therapy not performed. These patients may respond well to reperfusion therapy such as IV tPA or endovascular therapy. This mismatch condition is called "perfusion – core mismatch".
2) Penumbra
A cerebral infarction occurs when a cerebral arteries occludes. The brain cells in the central core of the infarction would be irreversible, but the area surrounded the core has a potential to recover and to be salvageable. These area are called the penumbra, and it is considered to regain its brain function depending on the salvageable treatment.
Cases for IVT and EVT at NCVC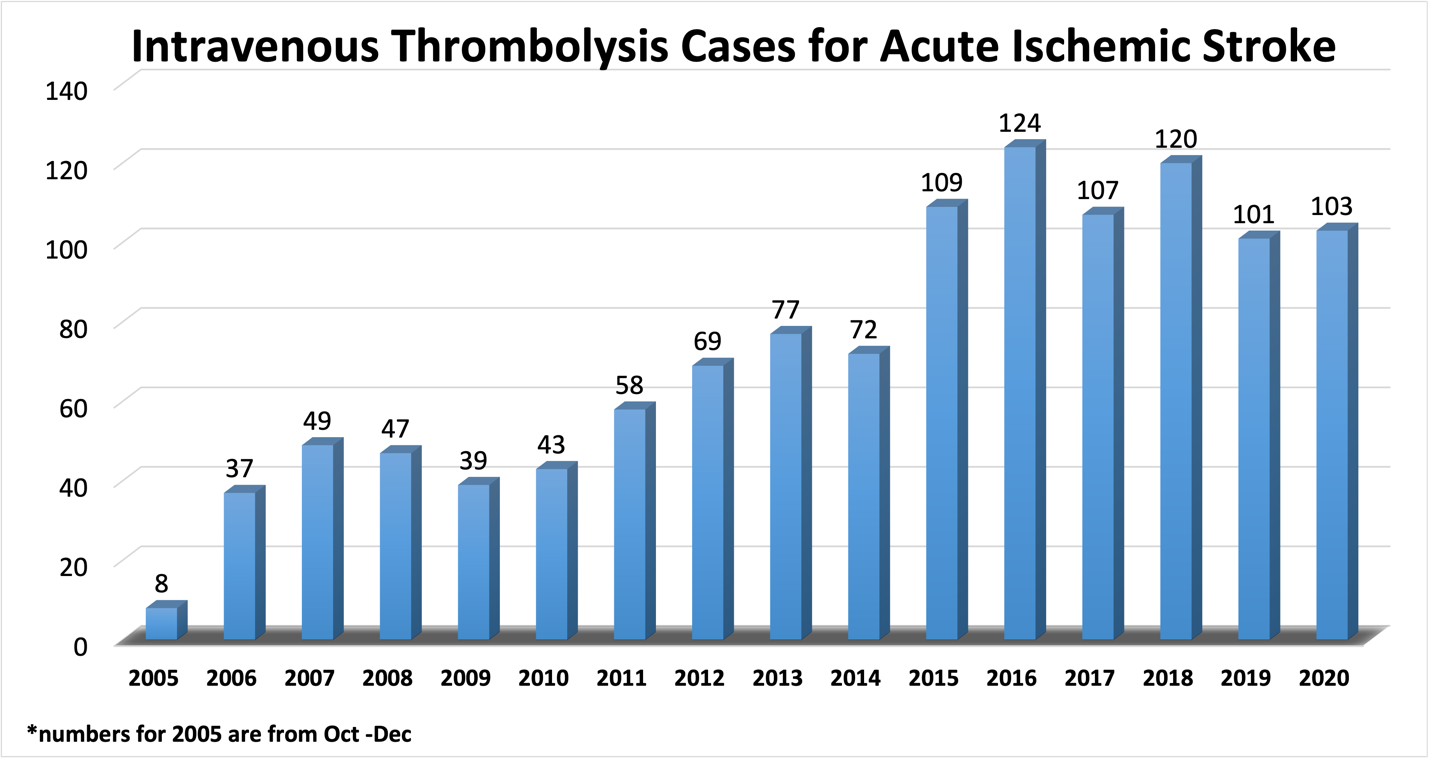
Intravenous tPA therapy can be used for early-onset ischemic stroke patients within 4.5 hours of onset. The earlier the treatment is started, the better the outcome can be expected. It is essential to start the treatment as soon as possible. An immediate visit to a specialized hospital by ambulance when a stroke is suspected will greatly contribute to the clinical outcomes.
From 2019, intravenous tPA therapy can be considered based on head imaging (e.g. mismatch between DWI and FLAIR imaging of MRI) even if the time of onset is not known or a wake -up stroke.
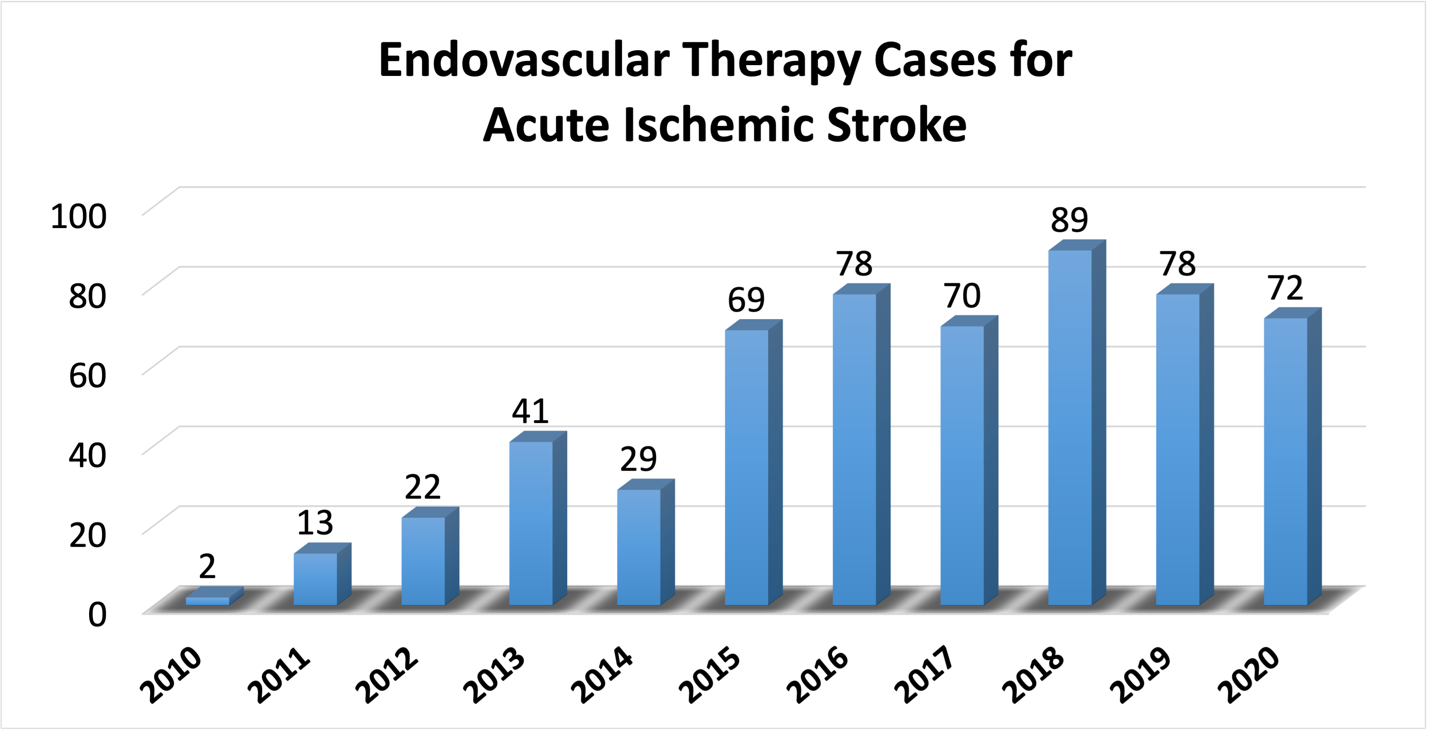
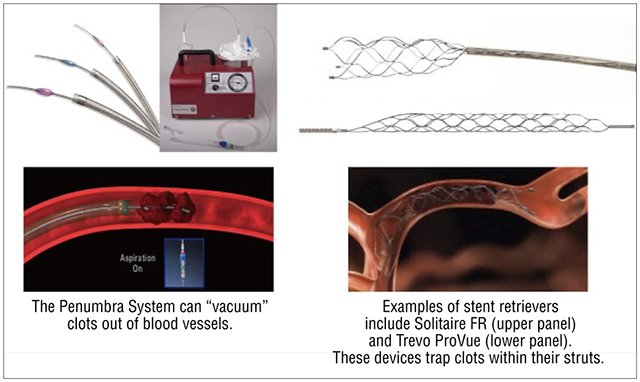
In addition, acute ischemic stroke within 8 hours of the onset (up to 24 hours in some cases when symptoms are slowly progressing analyzed by RAPID) and for who did not respond to intravenous tPA therapy well, the Merci Retrieval System was approved for endovascular treatment (catheterization) in October 2010, and from October 2011, the Penumbra System was approved for endovascular treatment (catheterization) to mechanically remove the blood clots. In addition, a stent-type clot retrieval device was approved in March 2014.
Endovascular treatment for acute ischemic stroke, bridging with intravenous tPA therapy, has been actively performed for patients who are eligible from its efficacy proved in 2015. At our hospital, three certified Japanese Society of Neuroendovascular physicians collaborating together with with Neurosurgeons, are carefully assessing patients who are eligible for EVT and proceeding to the treatment.
Please recognize the warning signs of stroke such as Face dropping, Arm weakness, Speech disability, and its Time to call 119 immediately (FAST). This can make the difference between a strong recovery and disability or even death.
Stroke Emergency Care
The first 4.5 hours after stroke onset is the optimal time window for acute treatment.
An acute stroke is a disease in which blocked blood flow leads to cerebral nerve damage. In treating an acute stroke, it is critical to recover from the reduced blood circulation as soon as possible. As a way to treat stroke, tissue plasminogen activator (tPA) is infused intravenously. This helps dissolve clots (thrombolysis) and restore blood flow.
Cerebral artery recanalization by thrombolytic therapy
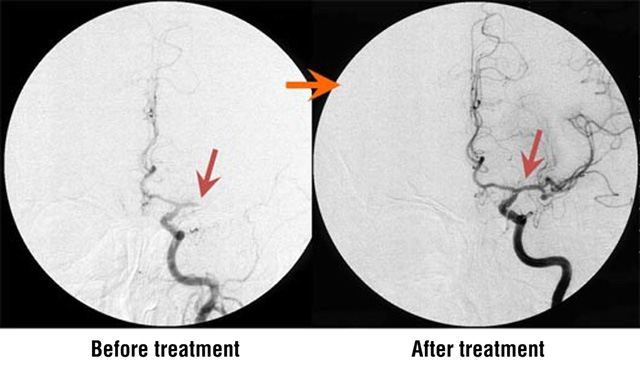
An embolic occlusion of the middle cerebral artery was the cause of cerebral infarction in this case. Thrombolytic therapy, such as intravenous tPA, was administered to recanalize the artery of concern. The photos above demonstrate the therapeutic effects of catheter-directed thrombolytic therapy.
Clinical outcomes of intravenous tPA therapy
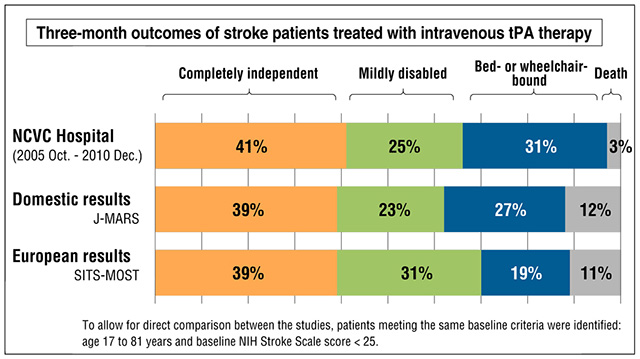
J-MARS, Japan Post-Marketing Altephase Registration Study; NCVC, National Cerebral and Cardiovascular Center; NIH, National Institutes of Health; SITS-MOST, Safe Implementation of Thrombolysis in Stroke-Monitoring Study.
Among patients treated at NCVC Hospital, 41% achieved complete independence (modified Rankin Scale score 0 or 1), and this rate was higher than J-MARS and SITS-MOST results (<40%).
In cooperation with local ambulance services, we established a comprehensive acute stroke management protocol. The clinical outcomes at NCVC Hospital are among the best in Japan. More than a decade has passed since the 2005 approval of intravenous tPA therapy for treating acute stroke. This therapy was administered in more than 60,000 patients nationwide, proving to be the standard treatment of choice.
Number of patients treated with tPA at NCVC Hospital
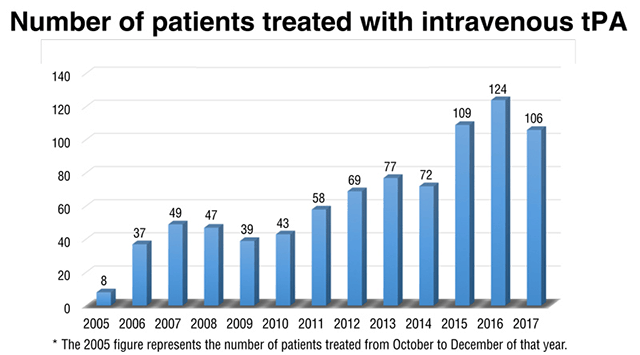
The time window for intravenous tPA therapy was extended from 3 to 4.5 hours in September 2012. A pivotal European study demonstrated the efficacy and safety of tPA administered within 4.5 hours of stroke onset, and this regimen was approved in many European countries in 2008. In Japan, extending the time window was approved at the end of August 2012.
The earlier thrombolytic therapy is administered, the better the outcome will be. Patients with acute stroke should receive medical attention as soon as possible. If you suspect symptoms of a stroke, call for an ambulance immediately and go to a specialty hospital.
Certain patients (e.g., those waking up with a stroke) are not sure when their symptoms began. We expect that head MRI examinations can identify patients for whom tPA is effective despite the absence of information about the amount of time elapsed since stroke onset. We are conducting a clinical trial to investigate the validity of this treatment modality.
Mechanical thrombectomy options are also available for patients with stoke who are not indicated for or responsive to tPA therapy. The Merci Retrieval System and the Penumbra System were approved as endovascular catheter devices for clot removal in October 2010 and October 2011, respectively (see figure below). Moreover, several stent retrievers were approved in 2014 (see figure below). Stent retrievers may yield better recanalization outcomes than other techniques. These thrombectomy modalities are generally indicated for patients within 8 hours of onset.
A series of clinical trials published in 2015 showed that endovascular therapies are as effective as intravenous tPA therapy for acute strokes. Based on these findings, we are actively using endovascular therapies in eligible patients. NCVC Hospital has four brain specialists and consultant specialists certified by the Japanese Society for Neuroendovascular Therapy (JSNET). In cooperation with the Division of Neurosurgery, they carefully evaluate options for the best outcome.
Endovascular treatments using the Penumbra System and stent retrievers
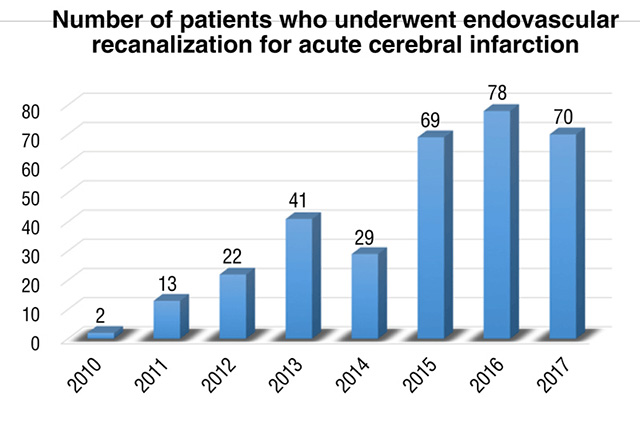
Number of patients who underwent endovascular recanalization for acute cerebral infarction
Even if more than 4.5 hours have passed since stroke onset, specialty care is still critical. Call for help immediately if you suspect a stroke has occurred.
Acute Stroke Unit Care and Rehabilitation
Excellent outcomes are still possible for patients presenting at NCVC Hospital more than 3 hours after stroke onset. The Stroke Care Unit (SCU) is dedicated to patients experiencing acute stroke and provides intensive medical treatments and acute rehabilitation programs. Even if more than 3 hours have passed since stroke onset, it is important that you receive specialized medical attention.
Resources for Health Care Professionals
- Visit Comprehensive superacute stroke care that includes intravenous tPA and endovascular therapies.
last updated : 2021/11/25
