Department of Pediatric Cardiology
More details
Advanced medical treatment at the Department of Pediatric Cardiology
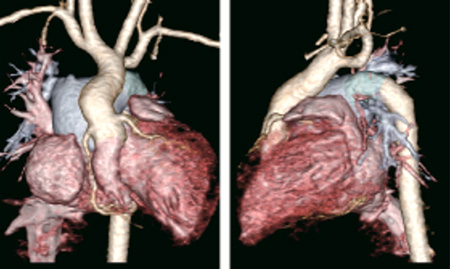
Diagnosis of heart diseases using imaging modalities
At the Department of Pediatric Cardiology, we actively use diagnostic modalities with advanced technologies. One of them is three-dimensional echocardiography; it allows three-dimensional reconstruction of echocardiographic images in real time, enabling accurate diagnosis of structural and functional abnormalities of the heart and great vessels. We perform approximately 200 examinations per year using this modality. In addition, we use transesophageal echocardiography, which involves the insertion of a gastroscopy camera-like fiber tube via the oral cavity to closely examine the heart through the esophagus, in approximately 360 patients per year. This modality is particularly effective in determining whether an atrial septal defect can be safely closed by catheterization. It also helps in effective evaluation of the cardiac function in postoperative patients, which is difficult to achieve using ordinary echocardiography. Furthermore, transesophageal echocardiography is used to observe the pulmonary veins, located behind the heart. Multislice computed tomography, which involves drip injection of a contrast medium, generates approximate three-dimensional representations of the structure of the heart and great vessels. We use this modality for over 200 cases per year. Multislice computed tomography equipment and image processing technologies have been continually improving.
Catheter-based approaches for the diagnosis of congenital heart diseases
Catheter-based therapeutic approaches, which are less invasive than the conventional surgery, have rapidly improved recently, thanks to technological advancements. Currently, certain heart diseases, such as atrial septal defect, patent ductus arteriosus, and pulmonary valve stenosis, are treated almost exclusively with catheterization. The NCVC was the first advanced medical institution in Japan to actively adopt catheter-based procedures for the treatment of many cases. As a pioneering medical center that assumes the educator role for other medical facilities in the country, we have since gained extensive clinical experience and achieved successful outcomes, contributing to the enhancement of safety in medical care and dissemination of new treatment methods. Catheter-based therapeutic approaches are actively applied not only to pediatric patients but also to many adult patients. The number of cases treated with catheterization exceeds 250 per year, the highest number in Japan.
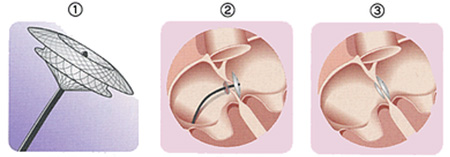
- A folding umbrella-like device is attached to the tip of a catheter for insertion.
- The device is fixed at the location of the atrial septal defect.
- The defect is closed.
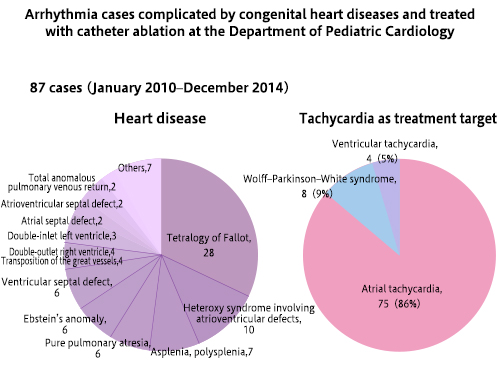
Diagnosis and treatment of arrhythmia
Arrhythmia that proves problematic in childhood can be divided into two types: bradycardia (slow pulse) and tachycardia (quick pulse). Treatment approaches vary depending on whether the patient has organic heart disease, such as congenital structural abnormality and cardiomyopathy (in which cardiac muscles are affected). At the Department of Pediatric Cardiology, we treat a broad range of patients with arrhythmia, regardless of the presence or absence of organic heart disease. Specific treatment methods include pacemaker implantation and management for bradycardia and administration of antiarrhythmic drugs and catheter ablation for tachycardia. For patients with organic heart disease, we first investigate the potential causes of arrhythmia to reduce the burden on the heart and eliminate the underlying cause while simultaneously providing care for bradycardia or tachycardia.
Exercise tolerance test and management of heart failure for patients with congenital heart diseases
Recently, there has been an increase in the number of adult patients with congenital heart diseases. For improved long-term prognosis and a better quality of life in these patients, accurate monitoring of cardiovascular dynamics is necessary, and it should be reinforced with comprehensive health management covering the respiratory function in patients with heart failure as well as monitoring their blood profile, liver and kidney functions, and overall metabolism. To improve the quality of life in late postoperative patients with congenital heart diseases, we strive to ensure high-quality diagnosis and treatment. In addition to using echocardiography and catheterization for diagnosis, we conduct cardiopulmonary exercise, respiratory function, and gastric function tests. Exercise tests are particularly effective in gauging the overall condition of a patient; we perform approximately 800 exercise tests per year, the highest number in Japan. In half of these cases, we also measure oxygen consumption as well as oxygen saturation during exercise, if needed, to obtain data useful for treatment.
Diagnosis and treatment of pulmonary circulatory diseases
Primary pulmonary hypertension is a rare disorder characterized by right heart failure due to a significant rise in pulmonary arterial pressure (about 30 pediatric cases reported per year in Japan). Without adequate diagnosis and treatment, the symptoms can rapidly worsen in children. We commenced treatment for primary pulmonary hypertension in 1979, looking after about 40 patients in total since then. Since 1999, when the administration of epoprostenol sodium (Flolan®) became possible, treatment outcomes at our department have considerably improved, and better therapeutic effects can be expected with the subsequent development of other drugs. At present, 30 pediatric and adolescent patients with primary pulmonary hypertension are being taken care of at our department and are being positively administered novel therapeutic agents. Additionally, many patients with other related diseases, such as Eisenmenger's syndrome and portopulmonary hypertension, and rare pulmonary circulatory diseases, such as pulmonary arterial aneurysm, are currently under our care. Furthermore, our efforts are focused on genetic analyses in collaboration with the Departments of Internal Medicine and Research Laboratories at the NCVC.
Nuclear medicine tests useful for various circulatory diseases
Nuclear medicine tests involve intravenous administration or inhalation of substances containing radioactive isotopes that emit weak gamma rays, enabling the evaluation of different aspects, such as morphology, function, and metabolism, of various organs. We perform approximately 400 nuclear medicine tests per year, primarily in patients with congenital heart diseases, pulmonary hypertension, Kawasaki disease, and cardiomyopathies, to evaluate cardiac muscle structure and function, pulmonary blood flow and ventilation, inflammation, and heart failure. Our department performs the highest number of nuclear medicine tests conducted in the area of pediatric cardiology in Japan. The ability of these tests to evaluate not only the heart but also the pulmonary circulation is critical for the diagnosis and treatment of complex congenital heart diseases. In fact, nuclear medicine tests are becoming increasingly important in the evaluation of cardiac function in adult patients with congenital heart diseases because these tests can be performed in patients who cannot tolerate other modalities, such as catheter examination and cardiac magnetic resonance imaging, due to allergy to an imaging agent, presence of a pacemaker, or other reasons. In 2013, we performed 403 cardiac nuclear medicine tests, including 140 myocardial and 136 pulmonary scintigraphies, which respectively accounted for approximately 35% of the total number of cardiac nuclear medicine tests performed.
Types of nuclear medicine tests
Myocardial scintigraphy: at rest, with exercise stress, and with medication stress
In myocardial scintigraphy, a radionuclide that accumulates in parts of cardiac muscles with blood flow is intravenously injected to evaluate ischemia in these muscles. In principle, an ergometer (an exercise machine) is used to induce stress, but medication may be used for primary school-age and younger children who cannot use an ergometer due to their body size.
Previously, thallium chloride was used as the radionuclide in these patients. Currently, however, we use 99m technetium in almost all tests because of its shorter half-life, which reduces the radiation dose. The imaging evaluation for congenital heart diseases is performed by pediatric cardiologists in collaboration with radiologists.
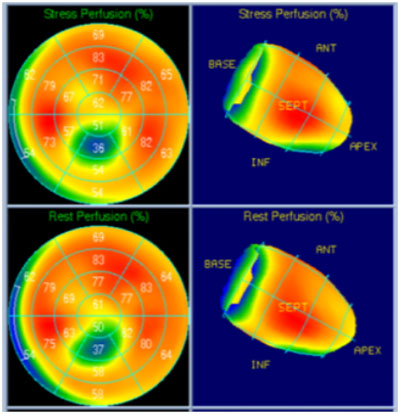
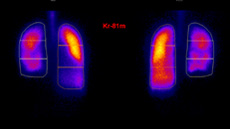
The upper panel images were captured after inducing stress; the lower-panel images were captured with the patient at rest. In this case, ischemia can be observed extending from the cardiac apex to the lower wall.
Pulmonary blood flow scintigraphy
Intravenous injection of a substance that accumulates in capillary blood vessels enables the illustration of the distribution of pulmonary blood flow between the right and left lungs as well as of the segments with hypoperfusion. This modality primarily helps determine treatment strategies for patients with certain diseases, such as cases of tetralogy of Fallot that tend to be complicated by pulmonary blood flow imbalance and regional hypoperfusion and cases of tetralogy of Fallot with major aortopulmonary collateral arteries. Pulmonary blood flow scintigraphy has been increasingly performed for the management of pre- and post-Fontan repair patients whose clinical condition is affected by the distribution of blood flow from the lower half of the body. This modality is also used to evaluate damage to pulmonary blood vessels due to pulmonary arterial hypertension.
Pulmonary ventilation scintigraphy
This modality involves inhalation of krypton gas (81mKr), followed by the evaluation of pulmonary segments where ventilation is occurring. Concurrent use of this modality with the abovementioned pulmonary blood flow scintigraphy enables the evaluation of imbalances in the ventilation/perfusion ratio. This modality can also be used for patients whose respiration and ventilation are affected due to scoliosis, postoperative phrenic nerve paralysis, or other reasons.
A representative case of ventilation/profusion imbalance Pulmonary ventilation scintigraphy and pulmonary blood flow scintigraphy were performed the same day for a patient. The left image reveals poor pulmonary ventilation in the right lung, whereas the right image reveals insufficient blood flow in the left lung.
<肺換気シンチグラム画像>
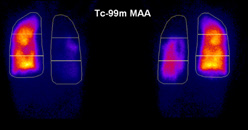
<肺血流シンチグラム画像>
We also perform other nuclear medicine tests, which provide valuable information that would otherwise be unattainable. These modalities facilitate not only patient evaluation but also treatment policy confirmation.
last updated : 2021/10/01
