Department of Pharmacy
To medicalstaff
Introduction
The mission of the National Cerebral and Cardiovascular Center is to provide education and training, as well as advanced pioneering medical care, and to produce leading medical professionals. The Department of Pharmacy promotes the proper use of drugs and drug therapy through drug management and instruction services. The department actively conducts research in clinical pharmacy, and collaborates with other hospitals and universities. To train pharmacists specialized in drug therapy for cardiovascular diseases, the department places emphasis on education and training: the residency system for pharmacists was introduced in 2010 and accepts pharmacists from the Japan Pharmacists Education Center or other facilities as well as students from pharmaceutical sciences departments of various universities.
Philosophy of the department
High levels of knowledge, skills, and a sense of ethics pertinent to drug therapy for cardiovascular diseases are applied to the provision of the optimum treatment and the advancement of medicine through research on therapeutic agents for the treatment of cardiovascular diseases and the dissemination of information.
Basic principles of the department
- We provide safe, reliable, high-quality, and highly specialized pharmacy services.
- We train pharmacists to play leading roles by providing information on recent advances in drug therapy for cardiovascular diseases.
- We promote clinical pharmacy research related to cardiovascular diseases.
- We disseminate information on drug therapy for cardiovascular diseases.
- We create an environment in which pharmacists can work with pride and a sense of accomplishment, and promote teamwork in health care.
☆Drug management and instruction services
The "drug management and instruction services"is a service by hospital pharmacists and introduced in April 1988 in response to the establishment of a new category of medical fees covered by Japanese national insurance termed "basic technical fee for inpatient dispensing"and the facility standard for its reimbursement. In April 2008, the introduction of an amendment to the medical service fee schedule led to the implementation of changes related to reimbursement, including the comprehensive evaluation of services provided to patients using high-risk drugs and patients with serious conditions requiring critical care hospitalization. For the latter patients, reimbursement for drug management and instruction services became possible even in cases in which instructions on the use of medications could not be provided directly to patients or if other types of drug management were implemented. The introduction of drug management and instruction services marked the transition from a service centered around outpatients to a service oriented toward inpatients. In addition, the service reflects the social demand for professional hospital pharmacists and the need for pharmacists to be part of the health care team.
The Department of Pharmacy began assigning pharmacists on duty to the general ward in April 2006. In April 2008, drug management and instruction services including assessment of drugs brought into the special ward by patients, the provision of drug information, therapeutic drug monitoring (TDM) of antimicrobial agents and antiarrhythmic agents, and monitoring of adverse reactions were started. Through these services, pharmacists contribute to ensure safety in medical practice and improve the quality of drug therapy as members of the medical care team (Table 1).
The amendment to the medical service fee schedule, adopted in April 2012, introduced an additional fee for pharmaceutical services provided in hospital wards (once a week, 100 points). The fee covers drug-related services provided by pharmacists at hospital wards to reduce the burden on other healthcare workers and improve the quality of drug therapy. At our center, this fee was introduced in May 2012.
In preparation for the move to the new hospital in July 2019, satellite pharmacies were newly established in all wards, allowing pharmacists to complete all ward drug duties and drug management guidance duties at the satellite pharmacy. This will bring doctors, nurses, and co-medical staff closer together, allowing for more active collaboration with other professions than ever before, and contributing to the enhancement of patient-centered team medical care and the proper use of medicines. Regarding team medical care, our center operates an AST (Antimicrobial Stewardship Team), ICT (Infection Control Team), NST (Nutrition Support Team), Pressure Ulcer Countermeasures Team, Palliative Care Team, Dementia Care Team, etc. Pharmacists are actively participating. In addition, we accompany the Department of Transplant Medicine and Diabetes and Lipid Metabolic Medicine to conferences and rounds, and participate in diabetes classes, kidney and hypertension classes, dyslipidemia classes, stroke classes, and cardiac rehabilitation classes for outpatients and inpatients. We carry out activities that lead to the understanding and prevention of cardiovascular diseases.
[Table 1. Changes in the frequency of drug management and instruction services]
| Mean number per month | Fiscal year 2020 | Fiscal year 2021 | Fiscal year 2022 |
|---|---|---|---|
| Number of cases for which a fee for drug management and instruction was calculated | 1,633 | 1,556 | 1,586 |
| Number of patients who received services | 1,319 | 1,318 | 1,433 |
In hospital wards with pharmacists on duty, the pharmacists meet with patients upon hospitalization, take inventory of the drugs brought by the patient, evaluate and collect information on these drugs, and provide physicians and other professionals with the corresponding information to prevent medical accidents.
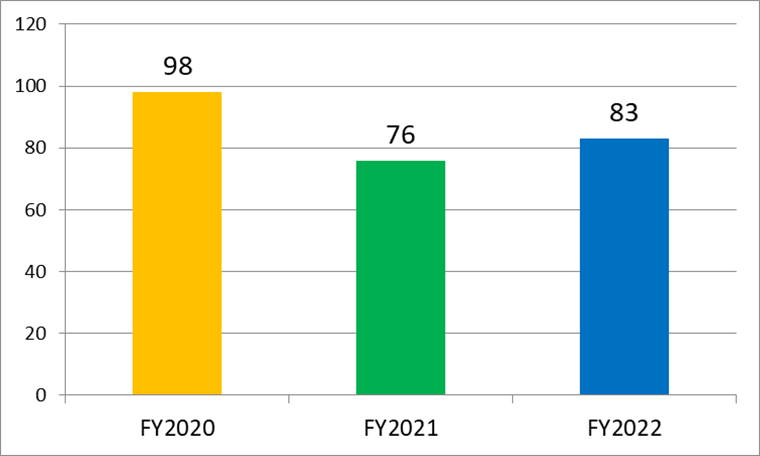
We established pharmacist-initiated systems for reporting the information on prevention and avoidance of adverse drug reactions, as well as drug safety. We contribute to safety in health care by formally reporting serious cases to the Japanese Society of Hospital Pharmacists and Pharmaceuticals and Medical Devices Agency (PMDA) (Figures 1 and 2).
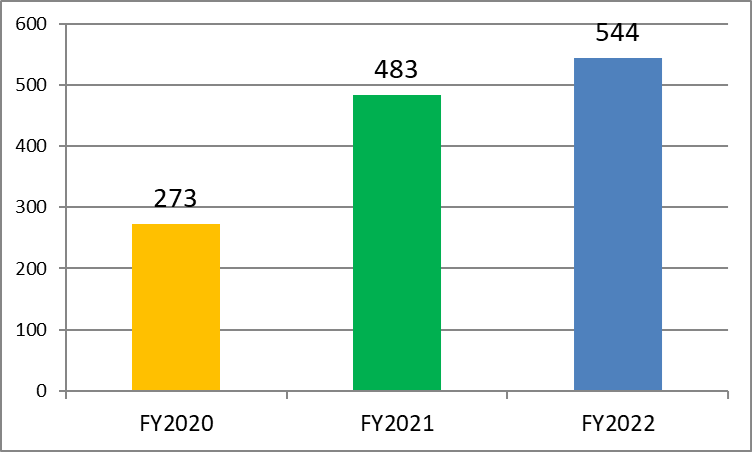
[Figure 2. Changes in the number of reports on adverse drug reactions]
In the hospital wards, pharmacists provide patients with information regarding drugs commonly used for different disease conditions by leading group discussions (Table 2).
[Table 2. Schedule for each classroom in the outpatient/in-patient]
| Classroom | Date and time to hold |
|---|---|
| Outpatient | |
| Hypertension | Once a month (11:00-12:00) The pharmacist gives a lecture for about 10 minutes.It rotates about once every two months. |
| Renal failure | |
| Diabetes | |
| Dyslipidemia | |
| In-patient | |
| Diabetes | Every Monday (13:00-14:00) |
| Kidney disease/hypertension | 1st, 3rd, 5th Friday (15:30-16:30) |
| Stroke | Second Wednesday (14:00-15:00) |
| Cardiac rehabilitation | Held irregularly once a month (12:45-13:30) |
☆Activities and roles of pharmacists in the healthcare team managing pre- and post-operative heart transplant patients
The Japanese Organ Transplantation Act was issued in October 1997, and the first heart transplant was performed in February 1999. By March 2010, more than 12 years after the enactment, 70 heart transplants had been performed. The Act for Partial Revision of the Act on Organ Transplantation (an amendment of the Organ Transplantation Act) was issued on July 17, 2009 and partially enacted (prioritized donation to family) 6 months later on January 17, 2010, with full enactment taking place on July 17 of the same year. After the amendment, 657 heart transplants were performed in the period up to January 1, 2023. In total, 727 heart transplants have been performed to date. Currently, the number of organ donors is limited, and patients requiring a heart transplant wait for a long time. In patients with worsening heart failure, drug therapy, including the use of catecholamines, is no longer effective and patients require a ventricular assist device to maintain cardiac function. At the NCVC, patients waiting for a transplant and patients who underwent a transplant receive care from various professionals working as a team to ensure consistency of care at the hospital ward dedicated to patients with heart failure. Pharmacists are members of the team and play important roles (Figure 3).
[Figure 3. Medical care team for patients wearing a ventricular assist device and patients who underwent a heart transplant]
![[Figure 3. Medical care team for patients wearing a ventricular assist device and patients who underwent a heart transplant]](/hospital/section/pharmacy/images/pha_zu4.gif)
The main complications associated with the use of a ventricular assist device are wound infection at the insertion site, thromboembolism, bleeding, and arrhythmia associated with heart failure. Post-operative patients after heart transplant may suffer acute or chronic rejection and opportunistic infection. Pharmacists are involved in the treatment of infections by selecting the appropriate drugs and performing TDM to ensure an effective blood concentration of drugs. Pharmacists collaborate with the infection control team (ICT) of the hospital.
Warfarin is the drug of choice for the prevention and treatment of thromboembolism inside the pump. Warfarin interacts with many drugs and foods, and the interaction increases or decreases its efficacy, possibly leading to serious bleeding or embolism. Adequate understanding of the interactions of warfarin is important for adjusting the prescription. Pharmacists provide information regarding interactions between warfarin and other drugs, and provide pharmaceutical care to ensure proper function of the coagulation system. For the treatment of arrhythmia, pharmacists manage drugs including amiodarone by TDM to ensure their efficacy and prevent adverse reactions.
Marked loss of appetite may occur in association with the progression of heart failure. A decrease in the body mass index may be an indicator of a poor prognosis. Nutritional management is an important part of the care of patients with heart failure, and the significance of the nutritional support team is well recognized. Pharmacists in the nutritional support team participate in the design of nutritional care strategies by selecting appropriate infusion preparations. In patients who underwent heart transplant, preventing rejection associated with the poor efficacy of immunosuppressants and avoiding adverse reactions associated with excessive administration of these agents are important issues. The blood concentration of immunosuppressants needs to be carefully monitored. Pharmacists participate in designing of the prescriptions along with physicians by managing the drugs used after heart transplant, such as cyclosporine, tacrolimus, everolimus, and mycophenolate mofetil through TDM. Furthermore, pharmacists implement TDM to prevent and treat opportunistic infections in pre- and post-operative heart transplant patients.
Pharmacists are involved in many aspects of medical care by providing comprehensive pharmaceutical care in drug therapies before and after heart transplant. The expertise of pharmacists is essential for teamwork in medical care. Figure 4 lists the current roles of pharmacists in the medical care team that manages patients waiting for a heart transplant and those who underwent heart transplant at the NCVC.
[Figure 4. Roles of pharmacists in the medical care team managing patients waiting for a heart transplant and those who underwent heart transplant]
![[Figure 4. Roles of pharmacists in the medical care team managing patients waiting for a heart transplant and those who underwent heart transplant]](/hospital/section/pharmacy/images/pha_zu5.gif)
☆ Therapeutic Drug Monitoring (TDM)
TDM requires expertise in pharmaceutical sciences. TDM does not simply measure drug concentration. Rather, the blood concentration of drugs is analyzed based on pharmacokinetic theories and the results are used for planning of the administration. Drug therapy is therefore optimized in individual patients in terms of efficacy and safety, and the proper use of drugs is promoted.
TDM consists of measuring the blood concentration of drugs as requested by physicians for the following purposes: 1) diagnosis of adverse drug reactions or drug poisoning; 2) medication planning and dose adjustment; 3) confirmation of therapeutic effects; and 4) confirmation of compliance. When changes in pharmacokinetics related to pathophysiological changes in individual patients are predicted or interactions between drugs are predicted, pharmacists proactively provide advice regarding the timing of blood collection. Recent studies reported associations between genetic polymorphisms in drug-metabolizing enzymes and individual differences in the blood concentration of drugs, the efficacy of drugs, and the onset of adverse drug reactions. TDM plays an important role in individualized medicine. At our test lab, cardiovascular drugs such as antiarrhythmic agents, immunosuppressants, and antimicrobial agents used in transplantation medicine are measured and analyzed (Figures 5 and 6).
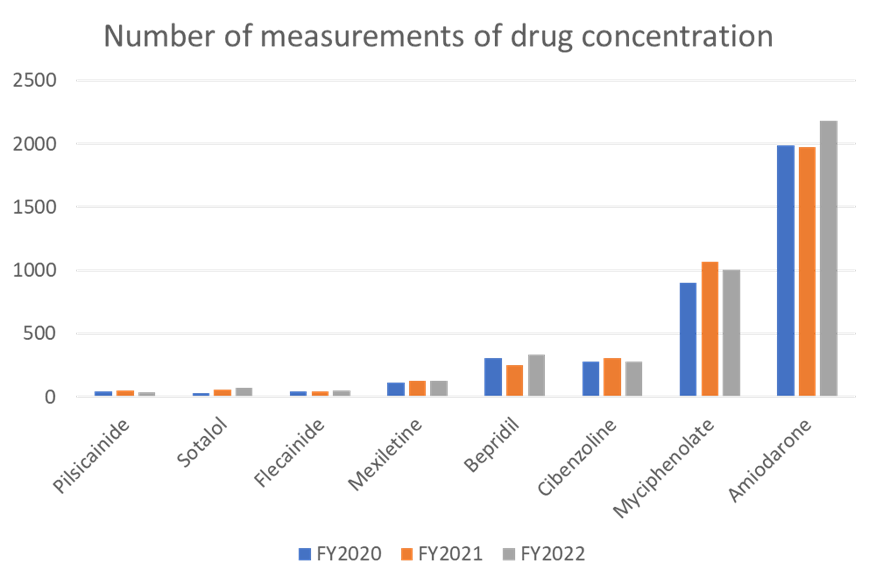
[Figure 5. Number of measurements of drug concentration]
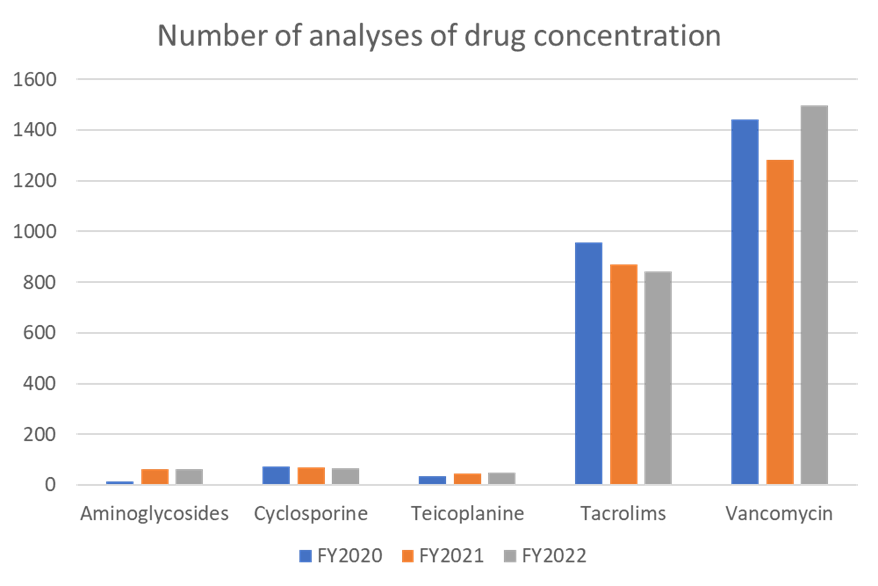
[Figure 6. Number of analyses of drug concentration]
last updated : 2024/01/10
