Department of Hypertension and Nephrology
To medicalstaff
Specialized information for healthcare professionals
Hypertension
At the Department of Hypertension and Nephrology, we determine treatment policies and evaluate the efficacy of antihypertensive therapies, both of which are based on the precise evaluation of patients' blood pressure data obtained after 24-hour monitoring and home measurements. Hypertension-related complications, such as arteriosclerosis and organ impairment, are carefully examined using ultrasound tests for the heart, kidneys, and blood vessels. Our diagnostic and treatment approaches for patients with secondary hypertension have led to positive results in many cases. For treating renovascular hypertension, we work in collaboration with the Departments of Radiology and Vascular Surgery to select the optimal treatment modality. The department is well experienced in the treatment of patients with particularly severe symptoms of hypertension, including malignant hypertension, who are often referred to as hypertensive emergencies.
Nephrology
For the diagnosis of kidney diseases, renal biopsy is performed in patients presenting with hematuria or proteinuria, and immunosuppressant therapies are administered when necessary. The causes of CKD are evaluated based on urine, blood, and imaging tests, and appropriate dietary and pharmacological therapies are administered to the patients. For patients with end-stage renal failure, arrangements are made to provide relevant education and to create arteriovenous shunts to ensure safety during dialysis.
1. Treatment of chronic renal failure
At the Department of Hypertension and Nephrology, we emphasize the following during the examination of patients with renal failure.
[1] Lifestyle improvement
A. Reduced salt intake: 3 g/day or more and below 6 g/day
B. Limited potassium intake: refrain from excessive consumption of fruits and vegetables
C. Smoking cessation
D. Weight loss: body mass index below 25 kg/m2
E. Moderate alcohol consumption
[2] Blood pressure management
Diabetics: below 130/80 mmHg
Non-diabetics with a positive proteinuria test: below 130/80 mmHg
Non-diabetics with a negative proteinuria test: below 140/90 mmHg
[3] Anemia management
Target hemoglobin level: 11 g/dl or above and below 13 g/dl
The hemoglobin level should not exceed 12 g/dl if medical history includes serious cardiovascular diseases and if complications are present.
[4] Management of hyperpotassemia and metabolic acidosis
Pay attention to the potential adverse effects of angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, and spironolactone as well as potassium intake through meals; assess for metabolic acidosis when potassium levels rise and in the loss of appetite
[5] Management of potassium/phosphorus metabolism
As CKD advances, a rise in phosphorus levels, a decrease in potassium levels, and an increase in parathyroid hormone production tend to occur. Priority should be given to the management of phosphorus and potassium levels.
[6] Lipid management
Low-density lipoprotein cholesterol: below 120 mg/dl (if possible, below 100 mg/dl); this is also for the prevention of cardiovascular diseases.
[7] Drug dosage regulation
As CKD advances, the dosages of drugs excreted via the kidneys must be reduced; moreover, the drugs should be administered at extended intervals.
2. Renal biopsy
The Department of Hypertension and Nephrology at the NCVC performs renal biopsies to screen for chronic glomerular nephritis, nephrotic syndrome, and renal impairment complicated by collagen disease to make a definitive histological diagnosis.
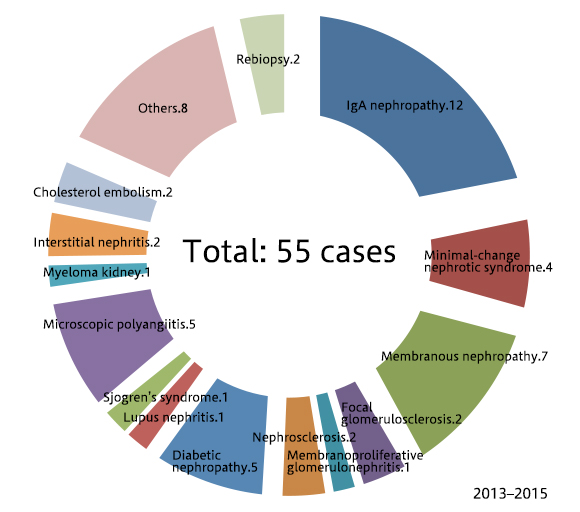
Below is a breakdown of the renal biopsies that we performed between 2013 and 2015:
| Total: 55 cases | |
|---|---|
| IgA nephropathy: 12 cases | Microscopic polyangiitis: 5 cases |
| Minimal-change nephrotic syndrome: 4 cases | Myeloma kidney: 1 case |
| Membranous nephropathy: 7 cases | Interstitial nephritis: 2 cases |
| Focal glomerulosclerosis: 2 cases | Cholesterol embolism: 2 cases |
| Membranoproliferative glomerulonephritis: 1 case | Others: 8 cases |
| Nephrosclerosis: 2 cases | Rebiopsy: 2 cases |
| Diabetic nephropathy: 5 cases | |
| Lupus nephritis: 1 case | |
| Sjogren's syndrome: 1 case | |
3. Introduction of tolvaptan (brand name, Samsca) for the treatment of polycystic kidney disease
Polycystic kidney disease (PKD) is an autosomal dominant disorder characterized by the development and growth of numerous cysts originating in the renal tubules of both kidneys due to a PKD gene mutation, causing rapid deterioration of renal function. Approximately half of the patients with PKD progress to the end-stage renal failure by the age of 70.Recently, the health insurance coverage of tolvaptan (brand name, Samsca), a vasopressin receptor antagonist, has been expanded to include PKD as an indication. Moreover, PKD has recently been added to the list of diseases recognized under the Act on Medical Care for Patients with Intractable/Rare Diseases of Japan. These developments have largely facilitated the introduction of tolvaptan for the treatment of patients with PKD.
Because the dosage of tolvaptan for treating PKD is considerably higher than that for treating heart failure or hepatic cirrhosis, strict management of patients' fluid intake and output is essential. At the Department of Hypertension and Nephrology, patients with PKD who are prescribed tolvaptan are first admitted to the NCVC Hospital for approximately one week to be instructed on the management of their water consumption and urination. This approach also ensures that they will not discontinue the medication on their own if they experience polyuria. The patients are also closely examined during their hospitalization to check for valvular heart disease and cerebral aneurysm, which can occur as complications in patients with PKD.
Because PKD is a genetic disease, the parents, siblings, and children of the patients are also screened for PKD. If they meet criteria for the prescription of tolvaptan, they are recommended to commence treatment to prevent CKD progression.
Patient referral and consultation
To refer your patients to the Department of Hypertension and Nephrology at the NCVC, first contact the NCVC's Specialty Care Coordinating Office.
Patients with hypertension are accepted at all times for a short hospitalization period for examination and education. Within a period of 3-7 days, patients undergo a battery of tests, including the evaluation of blood pressure, heart, kidneys, and blood vessels; the goals are to evaluate their cardiovascular system, introduce a dietary therapy, and allow them to attend classes on hypertension management.
For patients with kidney diseases, a 4-day biopsy hospitalization as well as a hospitalization period of 1-2 weeks for CKD education are available at all times. Patients can undergo dietary and pharmacological therapies as well as a range of physiological function tests and attend classes on CKD.
We encourage physicians to contact us for consultation concerning their practice and not only when facing difficulties in the treatment of their patients.
For the referral of patients with kidney diseases, our criteria for reception are as follows:
- Proteinuria: 0.50 g/gCre or above or 2+ or above
- Proteinuria and hematuria: both positive (1+ or above)
- Glomerular filtration rate < 50 ml/min/1.73 m2
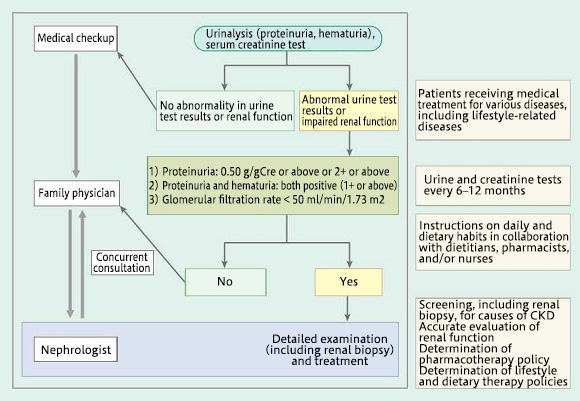
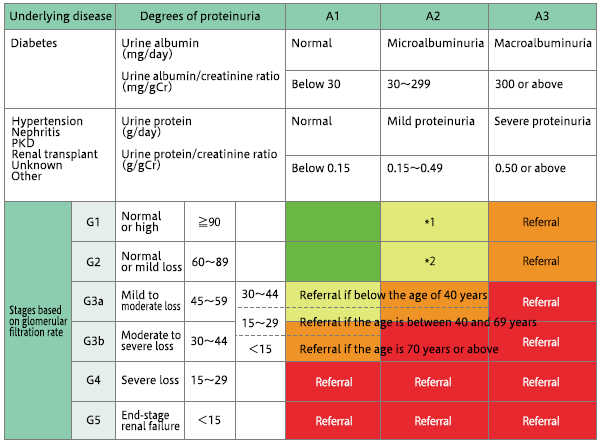
Immediate referral to a specialist is necessary for patients with 30% or greater deterioration of renal function within 3 months.
* Patients with simultaneous positive results for hematuria and proteinuria tests should be referred to the NCVC.
Clinical studies and research
The Department of Hypertension and Nephrology performs research on numerous topics, including home blood pressure-based tests for the treatment of hypertension, the efficacy of lifestyle improvements, antihypertensive drug-sensitive genes, and hypertension and cardiovascular disorders.
The department performs research on various topics in nephrology such as CKD and circulatory diseases, acute kidney injury, circulatory diseases in patients on dialysis, and fluctuations in body fluid levels and cardiac function during dialysis.
last updated : 2021/10/01
