Department of Transplantation
Target disease,treatment
Target diseases
The Department of Transplantation treats patients with severe heart diseases, such as those listed below, for whom conventional treatment modalities are unlikely to extend survival:
- Dilated cardiomyopathy
- Hypertrophic cardiomyopathy (dilated phase of hypertrophic cardiomyopathy)
- Constrictive cardiomyopathy
- Ischemic heart disease (ischemic cardiomyopathy following extensive myocardial infarction)
- Acute myocarditis (including fulminant myocarditis)
- Cardiac sarcoidosis
- Secondary cardiomyopathy in patients with muscular dystrophy
- Peripartum cardiomyopathy
- Incurable congenital heart diseases with cardiac failure
- Heart diseases (in patients aged <65 years) recognized by the Heart Transplant Suitability Subcommittee of the Japanese Circulation Society (*NB)
- The treatment options offered by the department includes heart transplant for patients with the diseases listed above.
(*NB) The page of the Heart Transplant Committee on the Japanese Circulation Society website (in Japanese):
http://www.j-circ.or.jp/hearttp/
Treatment modalities
Pharmacotherapies for heart failure
Optimal medication for each patient is selected on the basis of the department's abundant clinical experience from among the currently available pharmacotherapies for heart failure, such as beta-blockers, renin-angiotensin-aldosterone system inhibitors, diuretics, cardiotonic agents, phosphodiesterase 3 inhibitors, and carperitide (an alpha-human atrial natriuretic peptide).
Non-pharmacological therapies for heart failure
In collaboration with the physicians in the Division of Cardiovascular Internal Medicine who treat patients under their care, the Department of Transplantation selects and performs the most suitable treatment from among non-pharmacological therapies such as providing respiratory support and implanting pacemakers, including implantable cardioverter-defibrillator and cardiac resynchronization therapy-pacemaker or -defibrillator.
Intra-aortic balloon pump therapy and percutaneous cardiopulmonary support for conditions associated with cardiogenic shock syndrome
In collaboration with the cardiac intensive care unit of the NCVC Hospital, intra-aortic balloon pump therapy is performed and percutaneous cardiopulmonary support provided for mechanical circulatory assistance for patients presenting with cardiogenic shock syndrome. We are actively adopting these treatment modalities thanks to the availability of backup treatment with LVADs within the NCVC Hospital.
Treatment of conditions associated with cardiogenic shock syndrome using extracorporeal LVAD
LVAD implantation is selected as a "rescue"therapy (or a "bridge-to-recovery"therapy) for patients presenting with conditions associated with cardiogenic shock syndrome, such as fulminant myocarditis, peripartum cardiomyopathy, and extensive myocardial infarction.
In many cases of fulminant myocarditis, patients can expect recovery of their cardiac function. However, in most severe cases, wherein some of the cardiac functions are deteriorated over an extended period, LVAD implantation, which enables rapid evacuation of the left ventricle, is desirable because PCPS requires multiple transfusions and involves a reverse flow to upwardly flowing arteries, leading to the deterioration of the function of certain organ systems, notably the lungs, liver, and kidneys. In patients with peripartum cardiomyopathy, hybrid treatment combining LVAD implantation and bromocriptine administration is provided in collaboration with the Department of Perinatology and Gynecology.
Bridge-to-transplant therapy for chronic severe heart failure cases and other cases recognized as suitable for heart transplant
A battery of tests are performed in patients with chronic severe heart failure to examine their suitability for heart transplant. The committee charged with this evaluation within the NCVC examines the cases and registers patients deemed suitable as heart transplant candidates with the Japan Organ Transplant Network. In many cases, patients who are recognized as suitable candidates already suffer from advanced heart failure by the time their suitability is confirmed and require mechanical circulatory support. Therefore, upon the recognition of their suitability, patients are fitted with a continuous-flow LVAD, and education is provided to the patients and their families regarding at-home medical care. Patients are then released from the hospital and return home to wait for transplant.
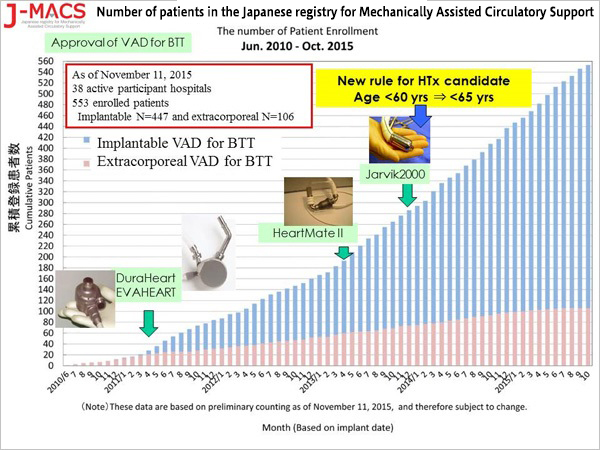
In April 2011, health insurance coverage was authorized for the continuous-flow ventricular assist devices DuraHeartTM and EVAHEART, which was later followed by the authorization for HeartMate IITM and Jarvik2000®. In 2013, the age limit for heart transplant suitability was raised to below 65 years. Consequently, the number of patients using VAD in Japan has increased over recent years (Fig. 1).
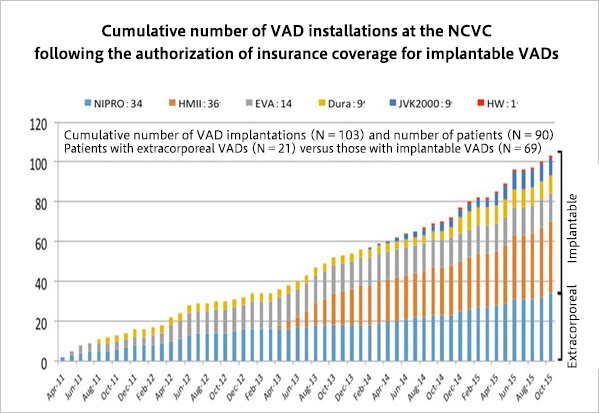
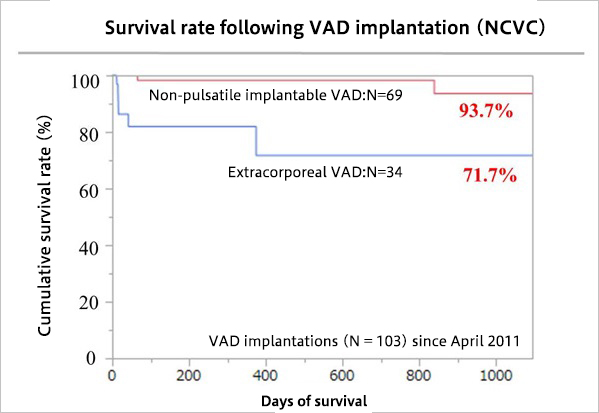
As a result, the number of VAD implantations has increased at the NCVC as well (Fig. 2). The outcomes of these implantations have been extremely favorable (Fig. 3).
Heart transplant
The Department of Transplantation performs heart transplant in collaboration with the Division of Cardiovascular Surgery. The department also provides postoperative care to patients with graft rejection and infection. Chronic-phase management includes various tests to evaluate the symptoms of rejection and administer and adjust the dose of immunosuppressant drugs. At present, the department has 80 heart transplant recipients under its care, including those who underwent the surgery outside Japan. Many of these patients have returned to an active life in society, including one patient who had undergone the transplant in Japan more than 15 years ago. The department organizes annual events where heart transplant recipients and healthcare professionals get together to provide support to the patients regarding various aspects of their lives. The events include CoCoRo-kai and summer camp for children who have undergone heart transplant.
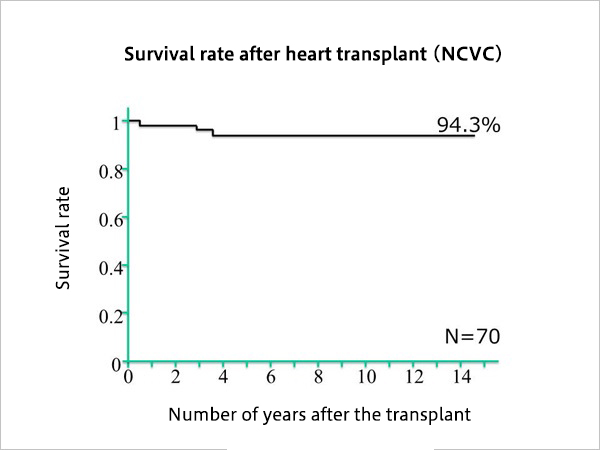
The survival rate after heart transplant is extremely favorable (Fig. 4).
last updated : 2022/07/27
