Department of Heart Failure
More details
- What is heart failure?
- Medication for heart failure
- Catheter-based treatment for structural heart diseases (SHDs) such as valvular disease and cardiomyopathy
- Catheter-based treatment for mitral regurgitation using the MitraClip®
- Catheter-based treatment for aortic stenosis: transcatheter aortic valve implantation (TAVI)
- Catheter-based treatment for hypertrophic obstructive cardiomyopathy: percutaneous transluminal septal myocardial ablation (PTSMA)
- Catheter-based treatment for mitral stenosis: percutaneous transseptal mitral commissurotomy (PTMC)
Developing future treatments
What is heart failure?
Heart failure is a condition that causes various symptoms due to reduced heart function. Major symptoms of heart failure are described below, although symptoms can vary by patient.
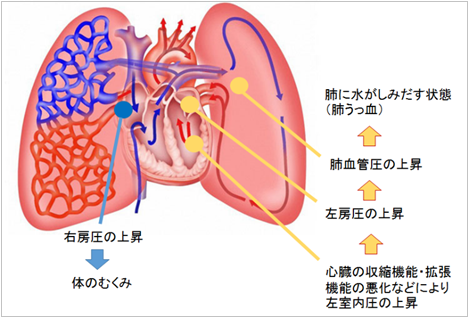
(1) Shortness of breath and respiratory discomfort
When the systolic and diastolic functions of the heart are persistently decreased, intracardiac pressure (left ventricular end-diastolic pressure) remains elevated, even in diastole. If this condition persists, pulmonary vascular pressure also rises and fluid exudes from the pulmonary blood vessels into the lung, resulting in lung congestion. In this situation, patients experience shortness of breath and respiratory discomfort. In the early stages, patients experience shortness of breath when climbing stairs or going up a slope. With disease progression, they will gradually start to experience shortness of breath even at rest. Finally, they will have difficulty lying down to sleep at night due to shortness of breath.
(2) Edema
Persistent elevation of intracardiac pressure leads to stagnation of blood flow into the heart and may cause edema in the legs.
(3) Tiredness and discomfort
Patients with severe heart failure may experience malaise and feel uncomfortable or sick due to an insufficient volume of blood being pumped by the heart.
The type and severity of symptoms vary by patient. Your condition is diagnosed based on your symptoms and also the results of several kinds of examinations. For details, please consult with your doctor.
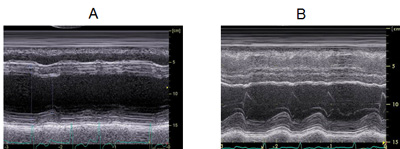
Medication for heart failure
Figure 1A shows a chest X-ray image of a patient who was admitted to the hospital because of shortness of breath due to heart failure. The heart is enlarged and fluid exudes into the lung, which is seen as a white shadow. The echocardiogram in Figure 2A shows that the heart is enlarged and its motion is compromised. For such patients, several medications are administered to eliminate the burden on the heart. After a patient's condition stabilizes, an oral medication called a beta-blocker is added. Beta-blockers are one representative type of medication for heart failure. It acts by slowing down the heart rate to rest the heart. Since these actions may cause a relapse of fluid retention in the lung, a beta-blocker is started at a low dose and carefully increased over several weeks. If patients are being effectively treated with medication, their heart size is reduced (Figure 1B) and the force of heart contractions is improved (Figure 2B). The effectiveness of beta-blockers varies by patient; it is evaluated based on symptoms and examinations such as echocardiography and blood tests. The following echocardiograms were obtained from a patient for whom medications were effective. The effectiveness of medications for heart failure varies from person to person. Medications are not necessarily effective for all patients with heart failure. The type and dose of medications are adjusted for individual patients based on their blood pressure, heart rate, symptoms, echocardiography findings, and blood test results.

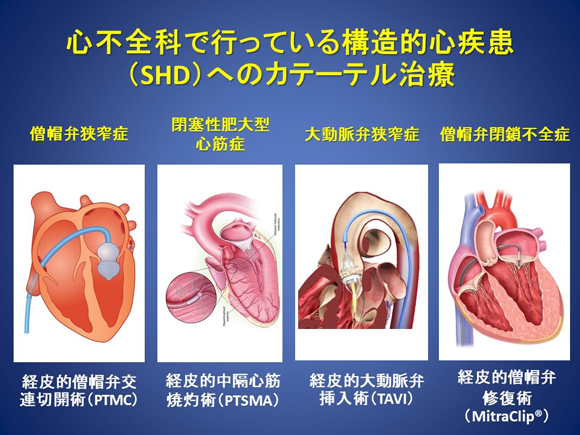
Catheter-based treatment for structural heart diseases (SHDs) such as valvular disease and cardiomyopathy
Age-related arteriosclerosis has become the primary cause of valvular disease. In Japan, which is becoming a super-aging society, the number of patients with valvular disease is continuously increasing (Figure 3).
Figure 3. Incidence of valvular disease by age and trends in population aging in Japan
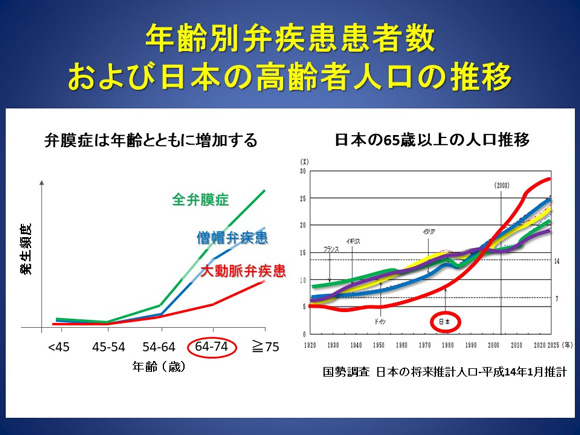
Although surgery has been the standard of care for valvular disease for many years, there are quite a few elderly patients for whom surgery is difficult or poses a high risk for complications. Recently, minimally invasive catheter-based treatments for specific diseases that can be performed in such high-risk patients have been developed and used in clinical settings. We perform catheter-based treatments for structure heart diseases (SHDs) such as valvular disease and cardiomyopathy. We have accumulated extensive experience in treating these diseases over many years (Figure 4).
Figure 4. Catheter-based treatments for structure heart diseases (SHDs) provided by the Division of Heart Failure

Catheter-based treatment for mitral regurgitation using the MitraClip®
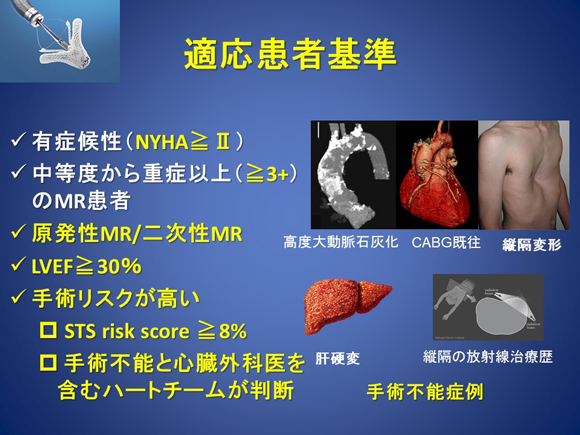
Mitral regurgitation is the most common valvular disease. In this condition, the mitral valve, which is a one-way valve, does not completely close. Consequently, blood is regurgitated from the left ventricle to the left atrium. It can be classified as primary or secondary. Primary mitral regurgitation is a condition in which the valve itself is broken. Secondary mitral regurgitation is a condition in which the part of the heart that holds the valve in place is enlarged due to heart failure or other reasons and a gap is created between the tips of the leaflets. In patients with secondary mitral regurgitation, invasive surgery is highly risky. It is usually not performed because it may worsen the disease due to regurgitation of the blood in many cases due to already-reduced cardiac function. Recently, the MitraClip® has become available for percutaneous catheter-based mitral repair (Figures 5-7). Many patients in Europe have already received this treatment. A clinical study was started in Japan, and the NCVC Hospital succeeded in providing the first case of this treatment in September 2015. Subsequently, we have performed the highest number of mitral repair procedures using the MitraClip® among the study sites in Japan.
The MitraClip® has been covered by public insurance since April 2018. NCVC Hospital is recognized as one of a small number of training facilities for MitraClip® procedures in Japan.
Animation of the MitraClip® procedure
The advantages of treatment with the MitraClip® include that 1) the procedure can be performed with the heart beating, without using cardiopulmonary bypass; 2) patients with renal failure can undergo the procedure because no contrast media is used; and 3) it is highly safe because a venous approach is used. Some patients with mitral regurgitation who are at high risk for open-heart surgery as well as elderly patients with mitral regurgitation may receive this treatment.
In particular, secondary mitral regurgitation is highly likely to be overlooked if echocardiography is not performed. It sometimes causes shortness of breath on exertion. In some cases, the severity of mitral regurgitation is moderate at rest but it becomes severe on exertion. We recommend that patients with shortness of breath who have been diagnosed with heart failure receive thorough evaluation that includes echocardiography and exercise echocardiography. At NCVC Hospital, experienced echocardiographers perform these examinations. If you are interested, please consult with our Valvular Disease Clinic at any time.
Figure 5. Percutaneous catheter-based mitral repair
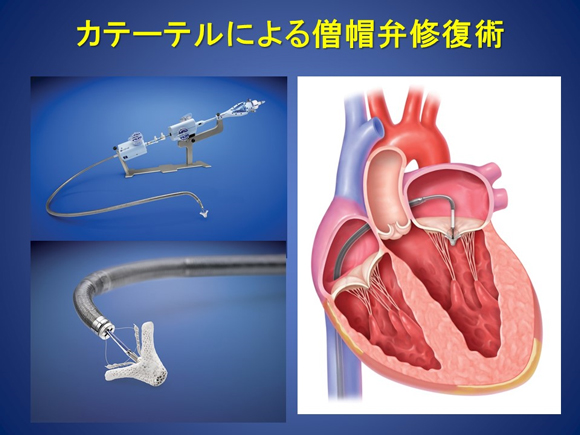
Figure 6. Number of MitraClip® procedures worldwide
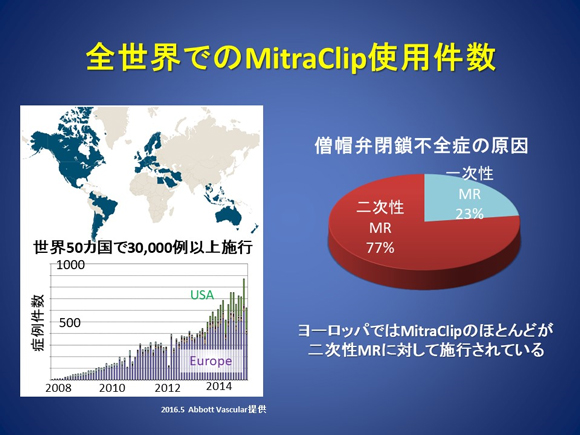
Figure 7. Eligibility criteria
Catheter-based treatment for aortic stenosis: transcatheter aortic valve implantation (TAVI)
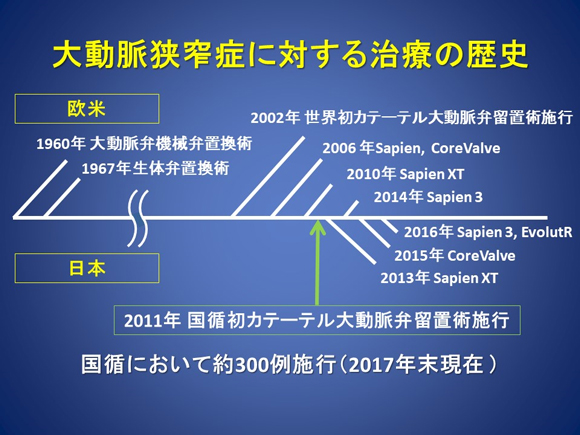
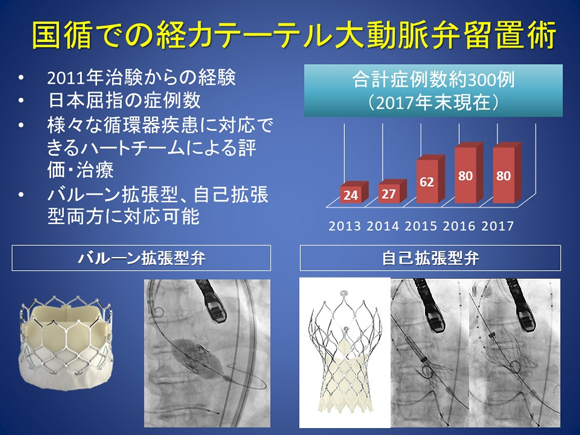
Aortic stenosis is a common valvular disease in elderly people that progresses over time. Without treatment, aortic stenosis has a very poor prognosis. Since transcatheter aortic valve implantation (TAVI) became covered by public insurance in 2013, patients who are high-risk surgical candidates have been able to receive implantation of a new bioprosthetic valve without open chest surgery.
At NCVC Hospital, we have accumulated experience in TAVI since the start of a clinical study in December 2011 (Figure 8). As of January 2018, NCVC Hospital has conducted approximately 300 TAVI procedures, one of the high volume center in Western Japan.
Figure 8. History of treatment for aortic stenosis
Both balloon-expandable valves and self-expanding valves can be used for TAVI (Figure 9). At NCVC Hospital, members of the heart team from various departments including cardiac surgeon, cardiologist, and anesthesiology thoroughly discuss and determine treatment strategies for each patient, including patient eligibility and device selection. We have a comprehensive system in place to address cases where emergent surgery is required. If you are interested, please visit our Valvular Disease Clinic for consultation.
- Click here for information on patient referrals
Figure 9. Transcatheter aortic valve implantation at NCVC Hospital
Catheter-based treatment for hypertrophic obstructive cardiomyopathy: percutaneous transluminal septal myocardial ablation (PTSMA)
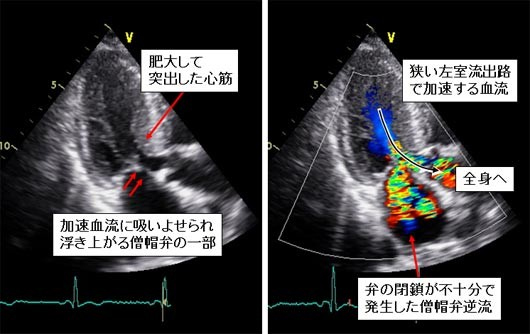
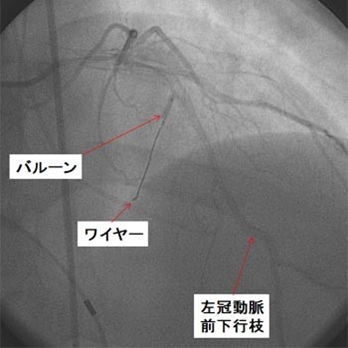
In some patients with hypertrophic cardiomyopathy, intracardiac pressure elevates to abnormally high levels due to thickened and prominent myocardium at the exit of the heart (Figure 10). In such cases, if a patient has severe symptoms and has risks of sudden cardiac death, surgery is considered to remove a part of the thickened myocardium. The same effect can be obtained by catheter-based treatment in some patients. The image on the lower panel in Figure 10 shows interventionalist inserting a wire into the vessel and selecting an arterial branch in a thickened part of the myocardium. In PTSMA, ethanol is injected into the target vessel and with the vessel blocked with a balloon to necrotize the thickened part of the myocardium. Several months after the procedure, the thickened part will be thinned, as seen after surgically resection of a part of the myocardium.
Figure 10
Catheter-based treatment for mitral stenosis: percutaneous transseptal mitral commissurotomy (PTMC)
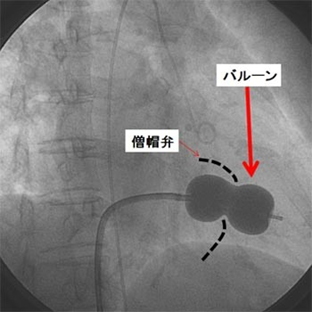
Once mitral stenosis progresses and blood flow is restricted, patients begin to experience shortness of breath and malaise on exertion. Although mitral stenosis is generally treated with open-heart surgery to replace the narrowed valve with a prosthetic valve, relatively mild cases may be treated by inflating a balloon attached to the tip of a catheter inside the narrowed valve (dotted line) to stretch it. After the valve has been stretched to a sufficient size, the balloon is folded up and retrieved (Figure 11).
Figure 11
Developing future treatments
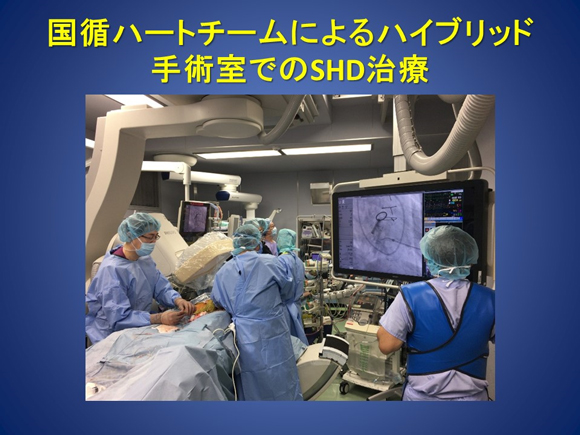
NCVC is committed to introducing advanced medical care and participating in numerous clinical studies to provide patients with leading-edge medical care in cooperation with the Department of Cardiovascular Surgery (Figures 12 and 13). Some treatments that could previously be provided only with an invasive approach are currently performed using minimally invasive approaches with a catheter in some overseas countries. We will introduce such minimally invasive approaches in Japan as soon as possible.
Figure 12. Clinical studies or trials of novel catheter-based treatments for SHDs in NCVC's Division of Heart Failure
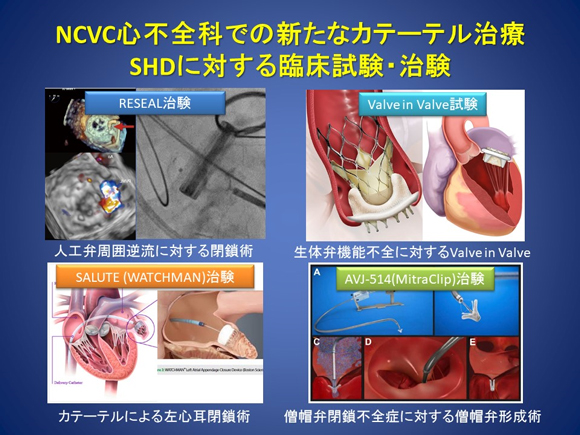
Figure 13. SHD treatment by the NCVC heart team in the hybrid operating room
Catheter-based treatment for prosthetic valve dysfunction
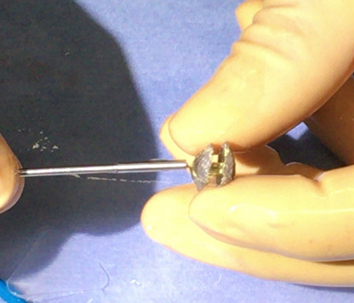
Paravalvular leak after valve replacement is a condition in which no prosthetic valve dysfunction is observed but backflow of the blood is observed around the prosthetic valve. Approximately 1% to 5% of patients with paravalvular leak develop severe hemolysis, heart failure, or both. Although surgery is the standard of care, it is highly risky because it is a repeat open-heart surgery and the tissues around the prosthetic valve are vulnerable. Overseas, it has been demonstrated that transcatheter closure is less risky and more effective than open-heart surgery. Transcatheter closure is performed after transesophageal echocardiography to examine the position, morphology, and size of the leaking areas (Figure 14). In this procedure, closure devices (Figure 15) are placed in the leaking areas under general anesthesia and transesophageal echocardiographic guidance to reduce backflow of the blood.
Figure 14
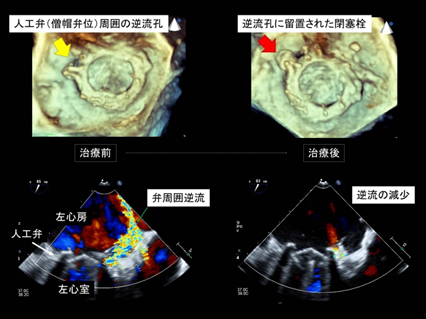
Figure 15
Bioprosthetic valves have lifetime of only a decade or so. They require repeat surgery due to deterioration approximately 15 years after placement. However, repeat surgery is highly risky and is likely to be difficult in elderly patients. For such patients, a valve-in-valve procedure, in which a second prosthetic valve is implanted within an existing prosthetic valve, has recently been performed in Europe and the United States. As with TAVI, a catheter is used to deliver the second prosthetic valve to the target site. At NCVC Hospital, we have obtained favorable outcomes with valve-in-valve procedures in patients who have previously received a prosthetic aortic or mitral valve (Figure 16).
Figure 16. Transcatheter valve-in-valve aortic valve implantation

last updated : 2023/04/05
