Division of Arrhythmia
Target disease,treatment
Conditions treated
Tachyarrhythmia
- Extrasystole
- Atrial fibrillation/flutter
- Paroxysmal supraventricular tachycardia
- Wolff-Parkinson-White syndrome
- Ventricular tachycardia
- Ventricular fibrillation
- Long QT syndrome
- Brugada syndrome
Bradyarrhythmia
- Sick sinus syndrome
- Atrioventricular block
Main diagnostic and therapeutic methods
Diagnostic methods
- Long-term (24-hour) Holter electrocardiography
- Exercise electrocardiography
- Signal-averaged electrocardiography
- Body surface potential mapping and magnetocardiography
- Electrophysiological testing
- Genetic diagnosis (long QT syndrome, Brugada syndrome)
Therapeutic methods
- Drug therapy for arrhythmia
- Percutaneous myocardial ablation (catheter ablation)
- Pacemaker implantation
- Implantable cardioverter-defibrillator (ICD) placement
- Ventricular resynchronization therapy (biventricular pacemaker implantation, cardiac resynchronization therapy [CRT], CRT with defibrillation [CRT-D])
- Removal of leads of implantable devices
- Arrhythmias you should fear and should not fear
- When you are told that you have arrhythmia
- Harmful arrhythmias and how they are treated
Photos or illustrations of the main therapeutic methods
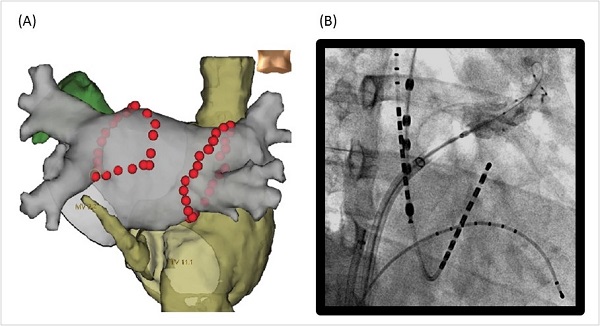
Catheter ablation is a method used to completely cure arrhythmia. Heat is applied to a part of the heart muscle by a high-frequency wave emitted from the tip of a thin tube (catheter) inserted into the heart. It causes a burn to remove the source of arrhythmia.
We are performing ablation using cutting-edge devices available due to advances in medical technology such as a three-dimensional mapping device that displays the shape of the heart in real time (Figure 1A) and irrigation catheters that are remarkably safe and effective. In recent years, we have also been performing catheter ablation for the treatment of atrial fibrillation using balloons (Figure 1B).
- Treating arrhythmia using ablation
- High-frequency catheter ablation therapy for atrial fibrillation (video)
In the video, catheter ablation is explained in an easy-to-understand manner.
Figure 1. Catheter ablation
Recent advances in implantable devices related to the treatment of arrhythmia are remarkable.
For current pacemakers, the main unit is implanted in the precordial area under the skin and connected through veins to the lead, which is placed in the heart. Recently, a clinical study of a leadless pacemaker has started. It has a smaller main unit implanted directly into the heart. The concept of pacemakers will dramatically change in the near future.
ICDs (Figure 2) are indispensable for patients with fatal arrhythmia. Their differentiation function, which reduces the occurrence of malfunctions, has been improved. The latest update about these devices is that subcutaneous ICDs (S-ICDs, Figure 3) have become available. S-ICDs have leads under the skin, not in veins or the heart. Therefore, it can be used in patients for whom previous ICD models could not be used because the lead could not be placed in a vein. S-ICDs are also expected to have a lower rate of serious complications associated with implantation surgery.
Furthermore, ICDs that can provide cardiac resynchronization therapy with biventricular pacing (CRT-D) have become available for patients with impaired cardiac function or symptoms of heart failure. These symptoms are often found in patients with indications for an ICD. Cardiac resynchronization therapy, which involves pacing using leads placed in the right atrium, right ventricle, and a branch of coronary sinus (Figure 4), is being established as an essential therapy for the management of severe heart failure.
We are also actively performing surgical lead removal using lasers, which does not require open heart surgery for patients who need it. Since 2010, it has been covered by insurance.
- Pacemakers and ICDs
- Surgical lead removal for implantable devices such as pacemakers
Many implantable devices for the treatment of arrhythmia are becoming compatible with magnetic resonance imaging (MRI). Previously, MRI was contraindicated after metal devices have been implanted. With new MRI-compatible devices, MRI is possible by resetting the program in advance when certain conditions are met.
In addition, many implantable devices are compatible with remote monitoring, in which information is sent from the patient's home. Remote monitoring enables early detection of device abnormalities or occurrences of arrhythmia. At our hospital, approximately 800 patients are currently monitored remotely.
In patients with no definite indication for ICD implantation or those who cannot undergo implantation immediately, wearable cardioverter-defibrillators can be used to prevent sudden death. This device requires patient understanding and cooperation. The maximum duration of use is 3 months. Furthermore, when patients tend to have syncope and it is unknown whether or not the syncope is caused by arrhythmia, an implantable loop recorder is useful for identifying the cause of the syncope. It is a stick-like device that fits in the palm (approximately 6 cm long). It is less invasive because implantation under the skin only requires local anesthesia; electrocardiograms can be monitored for as long as approximately 3 years using this device.
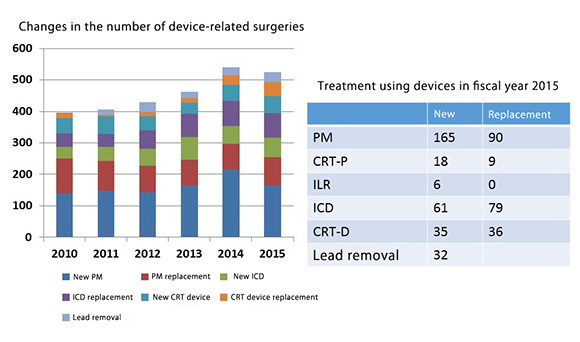
Figure 5 shows statistics about arrhythmia treatment at our hospital. We actively conduct clinical research on treatment using devices and publish data.
Figure 2. Radiograph after implantation of an implantable cardioverter-defibrillator
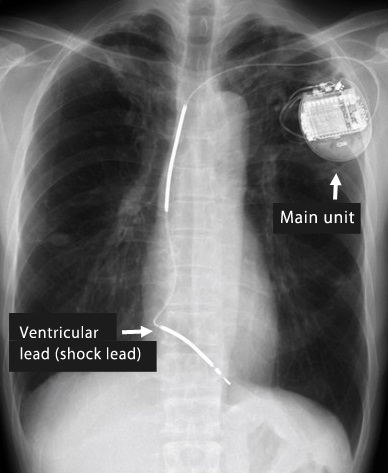
Figure 3. Subcutaneous implantable cardioverter-defibrillator
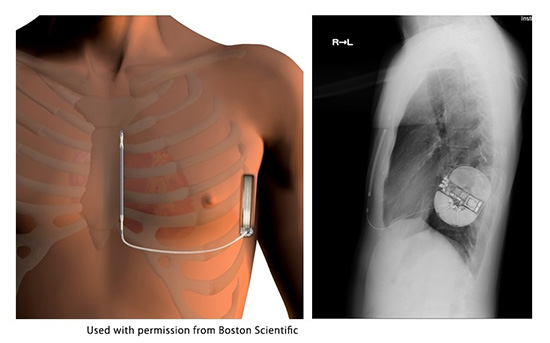
Figure 4. Radiographs showing cardiac resynchronization therapy
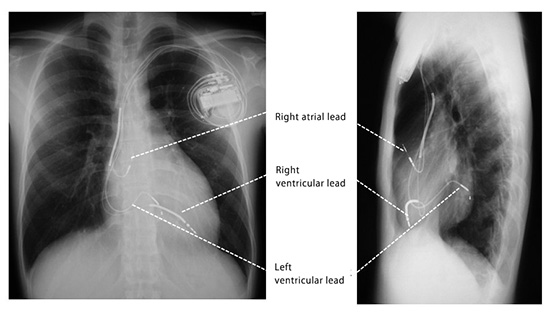
Figure 5. Statistics regarding treatment of arrhythmia using devices at our hospital
Major publications about devices
- Okamura H, et al. Initial experience using excimer laser for the extraction of chronically implanted pacemaker and implantable cardioverter defibrillator leads in Japanese patients. Journal of cardiology.2013;62:195-200
- Kamakura T, et al. Significance of non-type 1 anterior early repolarization in patients with inferolateral early repolarization syndrome. J Am Coll Cardiol. 2013 22;62:1610-8
- Takaya Y, et al. Electrocardiographic Predictors of Response to Cardiac Resynchronization Therapy in Patients With Intraventricular Conduction Delay. Circ J. 2014;78:71-7.
- Kamakura T, et al. Evaluation of the necessity for cardioverter-defibrillator implantation in elderly patients with Brugada syndrome. Circ Arrhythm Electrophysiol. 2015;8:785-91.
- Okamura H, et al. Risk stratification in patients with Brugada syndrome without previous cardiac arrest - prognostic value of combined risk factors. Circ J. 2015;79:310-7.
- Ishibashi K, et al. Improvement of cardiac function by increasing stimulus strength during left ventricular pacing in cardiac resynchronization therapy. Int Heat J. 2015;56:62-6.
last updated : 2021/10/01
